Endometrial hyperplasia (EH) is a condition in which the inner lining of the uterus becomes thicker and sometimes abnormal. There are different types of EH as viewed under a microscope, but the main difference between the benign and dangerous types is the presence of atypia.
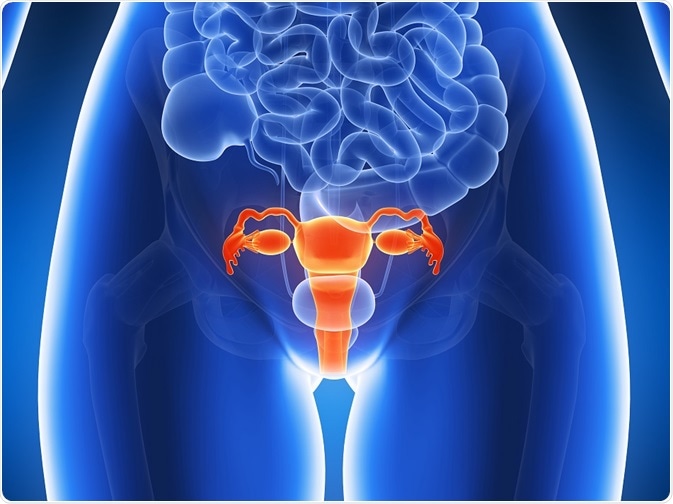
Credit: Sebastian Kaulitzki
Atypia refers to the presence of abnormal nuclear changes and cell alterations that signal the possibility or the actual presence of malignancy. Many studies have confirmed that up to 60% of women with atypical EH already have or are at a high risk of developing endometrial cancer of a well-differentiated type within a few years.
Risk factors
One study compared women with complex EH without atypia to other women with any other medical condition. Overall, the women with EH shared the following characteristics:
- They were more educated, with more than 12 years of education reflecting a risk of almost 3 times that in women with less than 7 years
- They were more likely to be obese, and obesity was associated with an almost threefold risk
- They had a higher rate of diabetes mellitus which was associated with almost 2.5 times higher risk
- They were unlikely to be postmenopausal, at which time the risk was 0.2 times that of the asymptomatic premenopausal woman
- If postmenopausal, the risk was increased 3 times if hormone replacement therapy (HRT) was being used
Other studies have identified the following risk factors:
- Age 45 years or below, risk 3 times higher
- Weight 90 kg or more, risk 5.5 times higher
- Infertility, risk 3.6 times higher
- Family history of cancer of the colon, risk 5 times higher
- Never having given birth, nulliparity, risk almost 3 times higher
Non-modifiable risk factors
- Caucasian origin
- Age 35 years or more
- Family history of EH, or of malignancy in the ovaries, breast or colon
- Lynch syndrome (hereditary non-polyposis colorectal cancer, HNPCC)
Menstrual factors
These factors have not all been confirmed in recent studies, but consist of:
- Postmenopausal status
- Prolonged interval between menarche and menopause, i.e., early menarche and late menopause
- A long perimenopausal period
Exogenous estrogen exposure
An earlier study identified the use of estrogen by postmenopausal women as a risk factor, with the risk increasing by more than 6.5 times. This went up to 20-fold if estrogen had been used for 5 or more years, but not if the estrogen came from an oral contraceptive preparation. In fact, these were associated with a protective effect against EH.
The Postmenopausal Estrogen/ Progestin Interventions (PEPI) trial studied just this single risk factor and found that treating postmenopausal women with 0.625 mg of conjugated equine estrogen for replacement therapy caused an almost 35% total increase in the risk of complex and atypical EH. This was not reduced by the addition of 2.5 mg medroxyprogesterone acetate.
Tamoxifen
The partial anti-estrogen drug tamoxifen has an estrogen-like proliferative effect on the endometrium. Prolonged use is associated with a higher risk of EH with the chances of endometrial cancer (a progression from atypical EH) being highly dose-dependent.
Chronic anovulation
On the other hand, obesity is often a part of the chronic anovulatory condition called polycystic ovarian syndrome (PCOS) which also comprises multiple ovarian cysts, hyperandrogenism, abnormal cholesterol levels, and diabetes mellitus. The peripheral fat deposits contain abundant aromatase enzyme reserves which rapidly convert the androgen androstenedione to estrone, and increase the estrogen levels in the blood. Chronic anovulation is also associated with a higher risk of EH.
Obesity
Along with obesity, modifiable risk factors associated with the genesis and maintenance of a high body mass index include:
- Sedentary lifestyle and the lack of exercise
- Poor dietary habits which make it easy to gain and difficult to lose weight
- Diabetes mellitus
If these are addressed by appropriate lifestyle changes, it is possible to target excessive estrogen production within the body and reduce it.
Tumors secreting estrogen
Another source of estrogen could be a functioning ovarian tumor such as a granulosa cell tumor.
Risk factors may also be classified as non-modifiable factors, factors related to the menstrual cycle, other medical conditions, estrogen-exposure related, and others.
Other risk factors
- Smoking
- Genetic mutations
Mechanism
All the data point in the direction of estrogen exposure, whether from within or outside the body, as a significant risk factor in the causation of EH. This can occur as a result of excessive ovarian production, or the conversion of androgens to estrogens within fatty tissue in overweight women, or the use of estrogen preparations.
It is noteworthy that the risk factors for EH with and without atypia are the same, but additional risk factors are used to predict when EH is likely to be precancerous. These include:
- Postmenopausal women, especially above the age of 53 years
- Diabetes mellitus
- Abnormal vaginal bleeding
- A body mass index (BMI) of 27 or higher
- Atypical EH – probably because of associated mutations in several genes linked to DNA repair and tumor suppressor genes, as well as unstable microsatellite areas. Many of these mutations are found in over half of endometrial cells from women with EH, and even more in cases of endometrial cancer.
Sources
- onlinelibrary.wiley.com/doi/10.1046/j.1525-1438.2002.01105.x/full
- https://www.ncbi.nlm.nih.gov/pubmed/10486458
- https://www.ncbi.nlm.nih.gov/pubmed/25041012
- https://www.ncbi.nlm.nih.gov/pubmed/3946378
- https://www.ncbi.nlm.nih.gov/pubmed/18514507
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4663224/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3573812/
- https://academic.oup.com/humupd/article/23/2/232/2632344
Further Reading
- All Endometrium Content
- What is Endometriosis?
- What Does the Uterus Do?
- Endometriosis Causes
- Diagnosis of endometrial hyperplasia
Last Updated: Feb 26, 2019

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article






