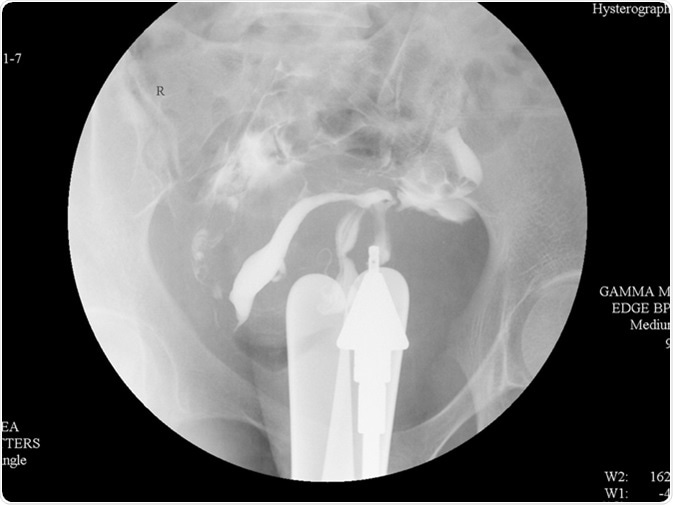
Hysterosalpingography is a hundred-year old diagnostic radiological technique which is used primarily to investigate female infertility. It is based upon the use of fluoroscopic screening of the uterus and the fallopian tubes as a radio-opaque contrast medium is flushed through them.
It is a widely-used and generally safe procedure if done under the right conditions. Following the introduction of fluoroscopic screening, complications have been drastically reduced. The controversy over whether to use oil-based or water-based contrast media for injection continues.
The Choice of Contrast Media
Oil-based media such as ethiodized oil were initially quite popular due to the finding that they improved fertility rates and brought down the time to conception. This research was not, however, duplicated by other studies, and as a result water-based and oil-based media were held to be of equal efficacy in hysterosalpingography.
Oil-based contrast did carry a certain risk of causing tubal granuloma formation in women who had damaged tubes, which led to its gradually falling out of favor. Water-based agents were held to be less caustic to the tubal mucosa. They do, however, cause more irritation to the peritoneal cavity following spillage, and distends the uterine cavity more rapidly, causing greater pain.
Furthermore, water-based contrasts are cheaper than the oil-based media, and they spread over the uterine and tubal contours more smoothly providing a better view. In addition, they are more likely to travel down the patent tubes fast, and are removed promptly from the peritoneal cavity. Also, they are less likely to be intravasated and, hence, to cause acute hypersensitivity reactions.
Very recent research reports that 40% of patients who had this procedure conceived within 6 months when ethiodized oil was used, compared to 29% with water-based media. This may change the approach to hysterosalpingography, especially since the use of fluoroscopy has led to the elimination of mortality connected with the procedure.
The Mechanisms of Improved Fertility
The mechanisms of improved fertility include:
- Washing out of debris from the tubes
- Breaking down of peritubal adhesions which block tubal mobility
- Reducing the phagocytic activity within the peritoneum and so decreasing sperm phagocytosis
- Stimulating tubal cilia and improving tubal function thereby
- Bacteriostatic effect on the mucous membranes of the tubes due to the iodine content
With all this in mind, this procedure is likely to be used still more widely for the diagnosis and treatment of female infertility. It can detect endometrial polyps, submucosal fibroids, tubal occlusion or peritubal adhesions, salpingitis isthmica nodosa, hydrosalpinx and tubal inflammation or infection, among others.
Indications
The procedure is used to assess the internal contour of the endometrial cavity and the fallopian tubes in:
- Infertile women, both with a history of recurrent miscarriage and otherwise
- Women with pelvic pain
- Congenital or acquired uterine anomalies including septa and adhesions or synechiae, as in Asherman’s syndrome
- Other conditions that could cause menorrhagia or irregular menstrual cycles, including polyps, fibroids, and adenomyosis
- As a baseline investigation before tubal or uterine corrective surgery
- Rarely, to assess the integrity of the uterine scar following a C-section, though this has been largely superseded by other imaging methods
- Rarely, to confirm successful restoration of tubal patency following surgical treatment, or tubal occlusion after a sterilization procedure
Contraindications
- The primary contraindication is pregnancy, for which reason the woman is asked to report on the second or third day after her periods end. This is within the follicular phase, and rules out the presence of a fertilized ovum within the uterus or tubes. In addition, a beta-HCG test is ordered to confirm the absence of pregnancy.
- Active pelvic infection is a high-risk factor for infection following this procedure and is therefore a contraindication.
- Recent surgery on the tubes or the uterus is also a contraindication due to the likelihood of uterine perforation or tubal rupture, or due to the weakness of the healing tissues. This includes recent dilatation and curettage.
- It is also not advised to perform this procedure during the menstrual period or immediately after it, due to the increased risk of intravasation of contrast with open uterine vessels.
- Hypersensitivity to contrast agents is obviously a contraindication to its use in this procedure.
- Active bleeding from the vagina and suspected malignancy are also contraindications to its performance.
Sources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3443271/
- https://radiopaedia.org/articles/hysterosalpingogram
- cursoenarm.net/…/36478?source=see_link
- http://pubs.rsna.org/doi/full/10.1148/rg.262055109
Further Reading
- All Hysterosalpingography Content
- What is Hysterosalpingography?
- Complications of Hysterosalpingography
- Technique and Precautions During Hysterosalpingography
Last Updated: Feb 26, 2019

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article






