Tests that analyze biomarkers are used during cancer management to guide treatment and provide information about patient prognosis. These tests are often performed on tissue biopsy samples that require invasive procedures and can lead to significant side effects. In a new article published in the Journal for ImmunoTherapy of Cancer, Moffitt Cancer Center researchers show that PET/CT images can be used to measure levels of the PD-L1 biomarker of non-small cell lung cancer (NSCLC) patients in a non-invasive manner and, in turn, predict a patient’s response to therapy.
Checkpoint inhibitors, drugs used to reactive the immune system by targeting the PD1/PD-L1 signaling pathway, are commonly used to treat patients with NSCLC. While this type of therapy has greatly improved patient outcomes, it only works for roughly half of this patient population. To avoid treating those who may not respond, checkpoint inhibitor therapy is often limited to patients whose surgical biopsy specimen is shown to express the PD-L1 biomarker. However, performing an invasive surgery is associated with inherent risks, and occasionally the biopsy sample is not adequate to perform diagnostic testing or the testing procedure itself may fail. Therefore, researchers are trying to develop alternative strategies to identify patients who should be treated with targeted agents such as checkpoint inhibitors.
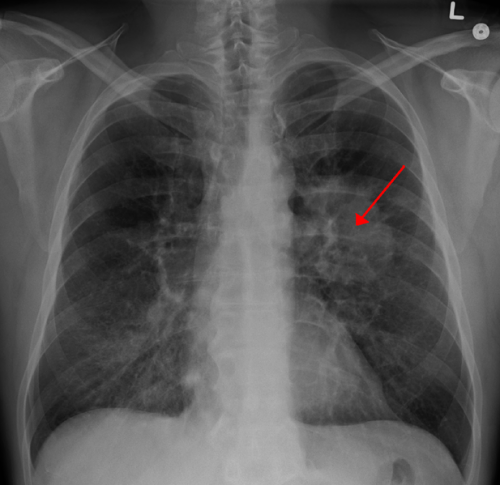
Moffitt researchers wanted to take advantage of the capabilities of computer deep learning to develop a new framework to measure PD-L1 biomarker levels in NSCLC patients in a non-invasive manner. They chose to use features of PET/CT scan images, such as shape, size, pixel intensity and textures to train computers to measure PD-L1 expression. They developed a deep learning score to predict PD-L1 expression, and after validation through different patient cohorts were able to use their model to predict checkpoint inhibitor outcomes in NSCLC patients.
“These data demonstrate the feasibility of using an alternative non-invasive approach to predict expression of PD-L1,” said Matthew Schabath, Ph.D., associate member of the Cancer Epidemiology Department. “This approach could help physicians determine optimum treatment strategies for their patients, especially when tissue samples are not available or when common testing approaches for PD-L1 fail.”
Source: Read Full Article






