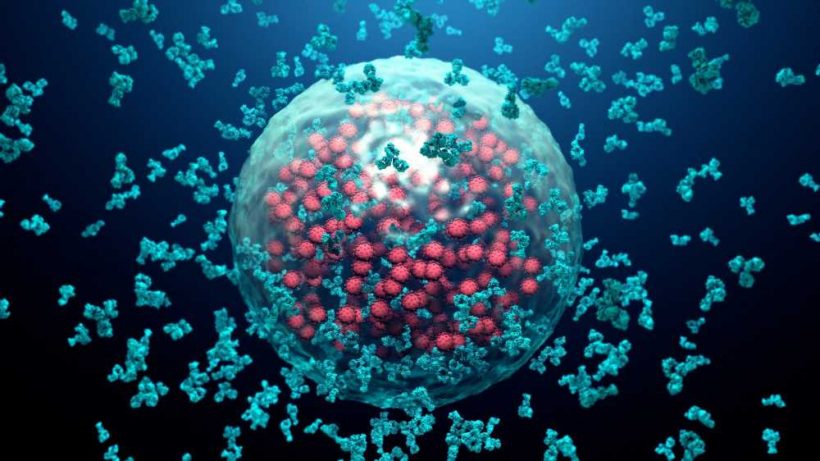
In a recent study posted to bioRxiv* preprint server, researchers at Ohio State University examined the degree of neutralizing antibody (nAb) evasion by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron XBB.1.5, CA.3.1, and CH.1.1 subvariants.
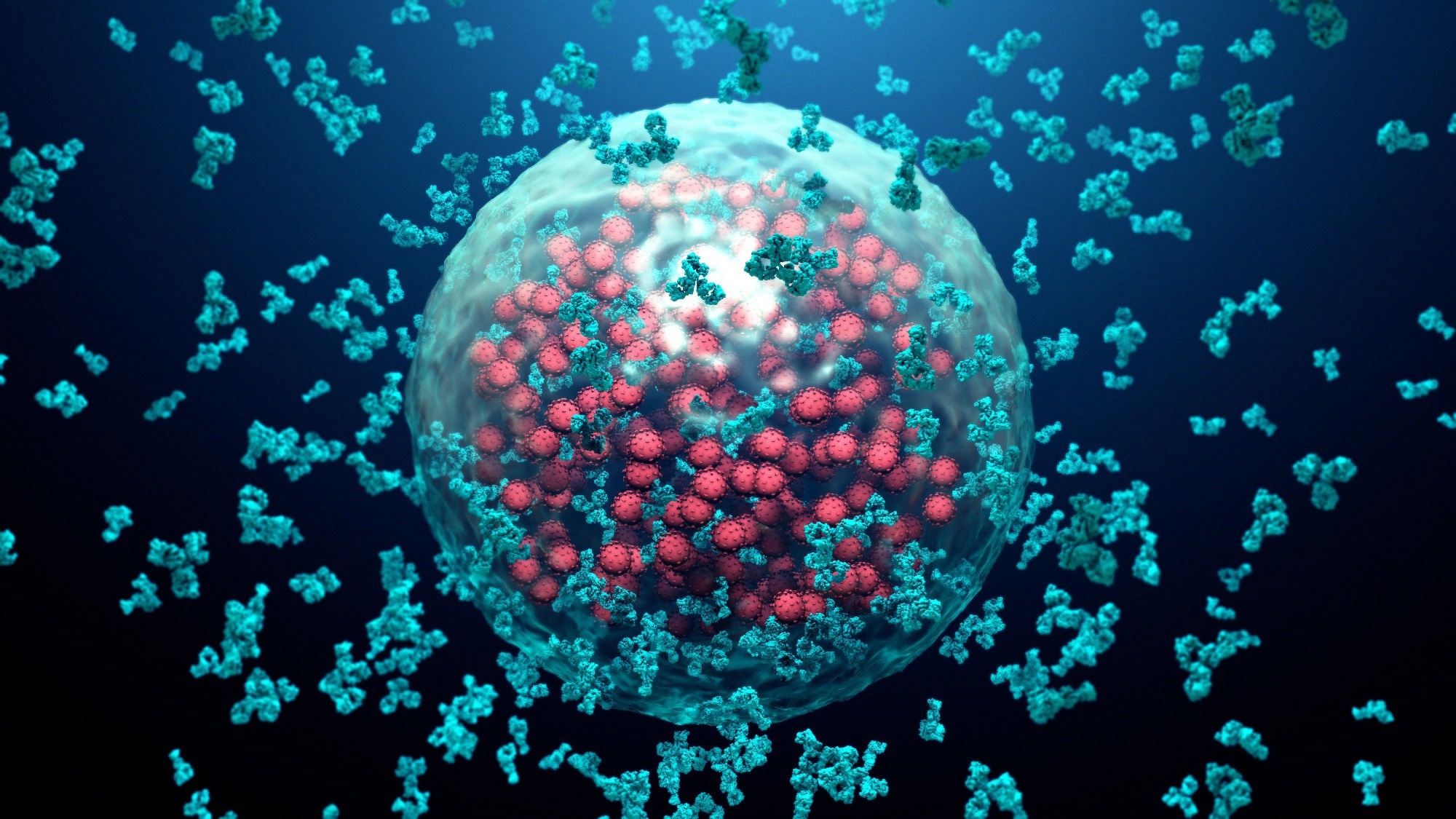 Study: Extraordinary Evasion of Neutralizing Antibody Response by Omicron XBB.1.5, CH.1.1 and CA.3.1 Variants. Image Credit: Design_Cells / Shutterstock
Study: Extraordinary Evasion of Neutralizing Antibody Response by Omicron XBB.1.5, CH.1.1 and CA.3.1 Variants. Image Credit: Design_Cells / Shutterstock
Several subvariants have emerged from SARS-CoV-2 Omicron, some showing relatively higher immune evasion, threatening vaccination efficacy. The BQ.1.1 sub-variant was the most prevalent following months of BA.5 predominance in the United States. Nonetheless, it is being quickly replaced by XBB.1.5. The XBB lineage was first detected in India as a recombinant of BA.2.75 and BA.2.10.1.1. Its emergence was alarming since it contained numerous mutations with established immune escape characteristics.
The effectiveness of monoclonal antibodies (mAbs), mono- or bivalent vaccines, and infection-induced immunity were reduced against XBB. The XBB lineage acquired two additional substitutions in the spike, resulting in XBB.1 and XBB.1.5 subvariants, and their impact remains unknown. In addition, the CA.3.1 and CH.1.1 subvariants of Omicron have been notable lately, as they carry the L452R substitution in the spike, previously discovered in the Delta and Omicron BA.4/5 variants.
The study and findings
In the present study, researchers evaluated the spike protein biology of emergent SARS-CoV-2 Omicron subvariants XBB.1.5, CA.3.1, and CH.1.1. First, they assessed the infectivity of spike-pseudotyped lentiviruses in HEK293T-ACE2 cells expressing human angiotensin-converting enzyme 2 (ACE2) and Calu-3 cell line. XBB.1 and XBB.1.5 had higher infectivity, with nearly two-fold increased titers than SARS-CoV-2 D614G in HEK293T-ACE2 cells.
XBB subvariants’ infectivity was not significantly different from that of D614G in this cell line. By contrast, CA.3.1 and CH.1.1 subvariants had nearly 2.5-fold lower infectivity than D614G in Calu-3. Next, the team tested neutralization of these emergent subvariants by sera from 14 healthcare workers (HCWs) boosted with a bivalent vaccine after two-to-four doses of monovalent mRNA vaccine.
Sera were obtained after a median of 66 days post-bivalent vaccination. CA.3.1, CH.1.1, and XBB.1.5 subvariants showed strong resistance to neutralization by sera relative to BA.4/5, with 4.6 to 17.7 times lower nAb titers than BA.4/5. Interestingly, XBB.1.5 had slightly higher nAb titers than its parent lineage (XBB).
Antibodies eBook
Of note, BQ.1.1 showed higher neutralization resistance than any of the XBB subvariants, with 12.8 lower nAb titers than BA.4/5. The CA.3.1 and CH.1.1 subvariants displayed much higher resistance to neutralization by bivalent sera. Next, the neutralization experiments were repeated using sera from HCWs vaccinated thrice with monovalent mRNA vaccines.
Samples were obtained after 2-13 weeks post-vaccination. The mean nAb titers of triple-vaccinated sera against SARS-CoV-2 D614 and Omicron (BA.2 and BA.4/5) were up to 5.6-fold lower than those of bivalent sera. nAb titers were markedly reduced for CA.3.1, CH.1.1, and XBB.1.5 subvariants. Overall, the trends of triple-vaccinated sera in neutralizing subvariants were comparable to those of bivalent sera.
In addition, the team examined the neutralization resistance of subvariants to sera from individuals infected with BA.4/5. They observed potent and near-complete neutralization resistance for CA.3.1, CH.1.1, and XBB.1.1 subvariants, with 2.6 to 4.1-fold lower nAb titers than BA.4/5. Furthermore, the researchers determined fusogenicity, surface expression, and processing of spike proteins of the subvariants.
Reduced syncytia formation was evident for all subvariants relative to D614G. XBB.1 and XBB.1.5 showed no differences in spike fusogenicity compared to XBB. The efficiency of syncytia formation of CA.3.1 and CH.1.1 was lower than BA.2.75.2. XBB subvariants, BQ.1.1, and BA.2.75.2 exhibited higher spike processing than D614G. There were no differences in spike processing for CA.3.1 and CH.1.1 subvariants relative to the parental BA.2.75.2.
Finally, homology modeling of XBB lineage spikes complexed with ACE2 or nAbs was performed. The P486 residue in XBB.1.5 was more hydrophobic than the S486 residue in XBB/XBB.1, resulting in favorable interactions with residues in ACE2, which allows better receptor utilization. The residue 486 is a hotspot for class I nAb recognition, and mutations at this site in XBB subvariants completely abolish interactions with the therapeutic mAb, AZD8895. Mutations at K444 and L452 residues found in CA.3.1 and CH.1.1 also affect interactions with class II nAbs.
Conclusions
Taken together, the findings suggested that bivalent mRNA vaccines induce up to eight times higher nAbs than monovalent vaccines. XBB subvariants, CA.3.1 and CH.1.1, exhibited almost complete escape from neutralization by triple-vaccinated or BA.4/5 infection sera. Moreover, XBB.1.5 did not show enhanced immune evasion relative to BQ.1.1. CA.3.1 and CH.1.1 subvariants consistently showed higher resistance to neutralization than XBB subvariants, warranting continued surveillance and further analyses.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Qu P, Faraone JN, Evans JP, et al. Extraordinary Evasion of Neutralizing Antibody Response by Omicron XBB.1.5, CH.1.1 and CA.3.1 Variants. bioRxiv, 2023, DOI: 10.1101/2023.01.16.524244, https://www.biorxiv.org/content/10.1101/2023.01.16.524244v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, Cell, Cell Line, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Enzyme, Healthcare, immunity, Omicron, Protein, Receptor, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Vaccine

Written by
Tarun Sai Lomte
Tarun is a writer based in Hyderabad, India. He has a Master’s degree in Biotechnology from the University of Hyderabad and is enthusiastic about scientific research. He enjoys reading research papers and literature reviews and is passionate about writing.
Source: Read Full Article