It’s expected that something without any monetary cost will experience greater demand than if there was an associated cost. However, the exact nature of the zero-price point has not been investigated outside of experimental trials until now. Researchers explored the “zero-price effect” of certain health care services in Japan. Variations in regional health care pricing structures gave the researchers a unique chance to study the real world consequences of zero pricing in health care. Their conclusions could inform health care providers on how to optimize their pricing, or non-pricing, of services to achieve certain strategic health care goals. The study is published in the American Economic Journal: Applied Economics.
Health care systems vary widely around the world. Even within countries there can be regional differences in the way health care services may be provided. For example in Japan, child health care services in some regions are completely free, in other regions there is a trivial fee, or copayment, equating to a few U.S. dollars, and in some regions, there is a small fee charged as a percentage of the insurance cost, or coinsurance. In all cases, the cost of child health care in Japan is extremely low, if not free, and this range of payment models presents a valuable opportunity for investigation by researchers studying the effect of zero pricing on health care.
“We tested the presence of a ‘zero-price effect,’ whether consumers demand disproportionally more if the price is zero instead of a very low price,” said Professor Hitoshi Shigeoka from the University of Tokyo’s Graduate School of Public Policy. “Prior studies in economics that examined the zero-price effect were limited to experimental settings or controlled laboratory experiments. We were fortunate that we could take advantage of the rapid expansion in subsidies for child health care in Japan over the last decade to identify the zero-price effect. To the best of our knowledge, this is the first study to credibly test the presence of the zero-price effect using real-world data.”
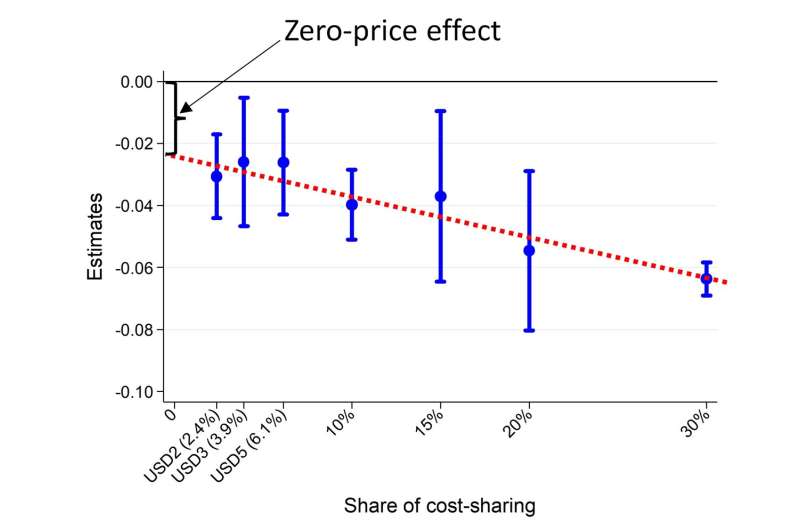
Shigeoka and his colleague Professor Toshiaki Iizuka from the Graduate School of Economics found that a zero-price effect, where demand at zero cost is not in line with demand at other, even trivially low prices, does indeed exist. They also determined that zero pricing can lead to poor allocation of health care resources by encouraging parents of healthier children to use more services, while parents of genuinely sicker children use no more or less services than when there is a small cost. Worryingly though, the researchers also found that a zero price can contribute to inappropriate overuse of antibiotics which adds to the increasing problem of antibiotic resistance.
“My advice for health service providers, health insurers, governments and policymakers, whoever is in charge of setting health care prices, is that they should recognize that a zero price is not just another price and use zero and nonzero prices strategically to achieve specific objectives,” said Shigeoka. “For example, the price for the COVID-19 vaccination should definitely be set at zero. But except for certain high-value care scenarios, the government should impose some small positive prices to reduce the overutilization of health care.”
Source: Read Full Article






