Parkinson’s disease has always been considered a brain disorder. However, new research reveals a close link between the disease and certain immune cells in the blood.
Researchers from Aarhus University have taken the first step on a path which can lead to new ways of understanding and, in the long term, possibly treating this widespread disease that affects not only motor functions but also cognition and emotions.
“We know that Parkinson’s disease is characterized by an inflammation in the brain, and that this is crucial for the progression of the disease. But in the study, our interest has been focused on the immune cells found outside the brain,” explains Marina Romero-Ramos, who is associate professor at the Department of Biomedicine at Aarhus University.
The researchers have studied a group of patients suffering from REM Sleep Behavior Disorder (RBD), a condition where the patients physically act vivid dreams with vocalizations and movements. If a patient e.g. dreams that they are running, their legs will move as if they were actually running. The sleep disorder is often discovered by a spouse as it results in violent movements at night, and the diagnosis is often indicative of something more. Patients with RBD have a high risk of developing Parkinson’s—statistically approximately ninety percent of them will be diagnosed with a parkinsonism related disorder over the course of five to 10 years.
The blood’s immune system changes very early on
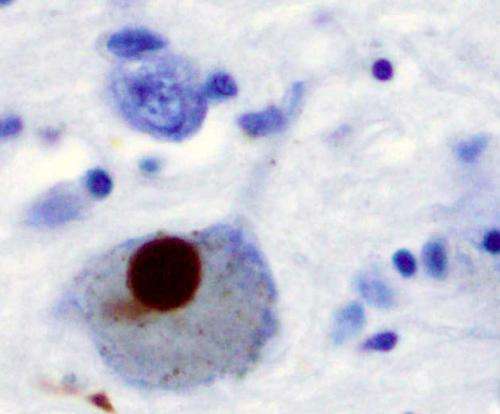
In Parkinson’s disease, a protein called alpha-synuclein aggregates in the neurons in the brain, and this kills the cells. The same protein also aggregates in the brain of people with the RBD, and it is therefore regarded as an early form of Parkinson’s disease. This has led the researchers from the Department of Biomedicine at Aarhus University—in collaboration with a group of neurologists and experts in nuclear medicine at Aarhus University Hospital, led by Dr. Nicola Pavese—to carry out scans of the brains of 15 patients with RBD and ten healthy people. The scan revealed that the patients with the sleep disorder had inflammation and a loss of neuronal activity in the brain. Although they did not present symptoms of Parkinson’s, their neurons were already ill and the brain’s immune cells were activated.
The groundbreaking discovery happened when Dr. Marina Romero-Ramos and her colleagues from Aarhus University analyzed blood samples from these patients. It turned out that the inflammation in the brain, and the associated loss of brain cells, directly related to changes in some immune cells in the blood, the monocytes. When certain proteins increased on these immune cells, there was in parallel increased inflammation in the brain and a decrease on the neuronal activity. This is a key finding when it comes to understanding Parkinson’s disease.
“We could see that the blood’s immune system changes very early on—even before Parkinson’s is diagnosed,” says Marina Romero-Ramos.
“This is the first study to show that the body’s immune system continuously communicates with the brain during the development of Parkinson’s disease, and that changes in the body’s immune system influence the condition of the neurons in the brain. In connection with Parkinson’s, this presents us with new opportunities for studying the immune cells in the blood and finding new forms of treatment,” she says.
This means that the researchers now hope to find and investigate ways to influence Parkinson’s disease by treating the blood and not the brain. Previous experiments on mice and rats suggest that this is possible, even though there is still much research to be done, as Dr. Romero-Ramos explains.
“This opens up the possibility of being able to design immunotherapy that modulates cells in the blood, which subsequently would stop or delay the changes in the brain. For the patients, being able to enjoy more years with good quality of life will be very significant,” she says.
“It also opens up opportunities for us to be able to find biomarkers in the blood that can tell us how someone’s brain is doing. Blood tests can be done more often and cheaper than a brain scan.”
Rare data from patients
The brain is a special type of tissue, and for many years researchers believed that the immune response in the brain was independent from the rest of the body. The study has now confirmed that the immune response in the brain and the body communicate with each other during RBD, and this is a discovery that the researchers could not have made without the help of the volunteers that took part in the study.
“We’ve had a unique combination of researchers at Aarhus University Hospital who take images of the brain, and researchers like me who analyze immune cells in the blood. It is very rare to get both analyzes from a patient and it has only been possible because a group of people were willing to participate in the trial, which we’re very grateful for. Participation involved two visits to the hospital for a brain scan, which itself isn’t painful, but of course it requires time and patience,” says Marina Romero-Ramos.
The data should be now evaluated and replicated by more labs, and hopefully new groups of patients will provide blood samples, brain scans and their patience for further testing.
Source: Read Full Article






