Are teicoplanin-non-susceptible Staphylococcus epidermidis strains increasing?
In a recent study published in the journal Scientific Reports, researchers elucidated the incidence patterns of teicoplanin-non-susceptible Staphylococcus epidermidis (Teico-NS S. epidermidis) over six years (2016-2021).
They examined the correlation between its occurrence and the annual utilization of teicoplanin.
Background
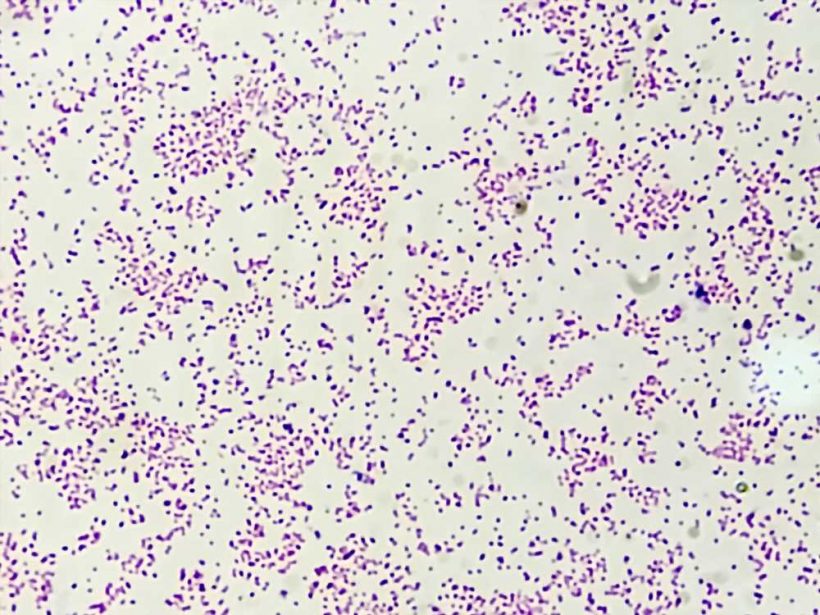
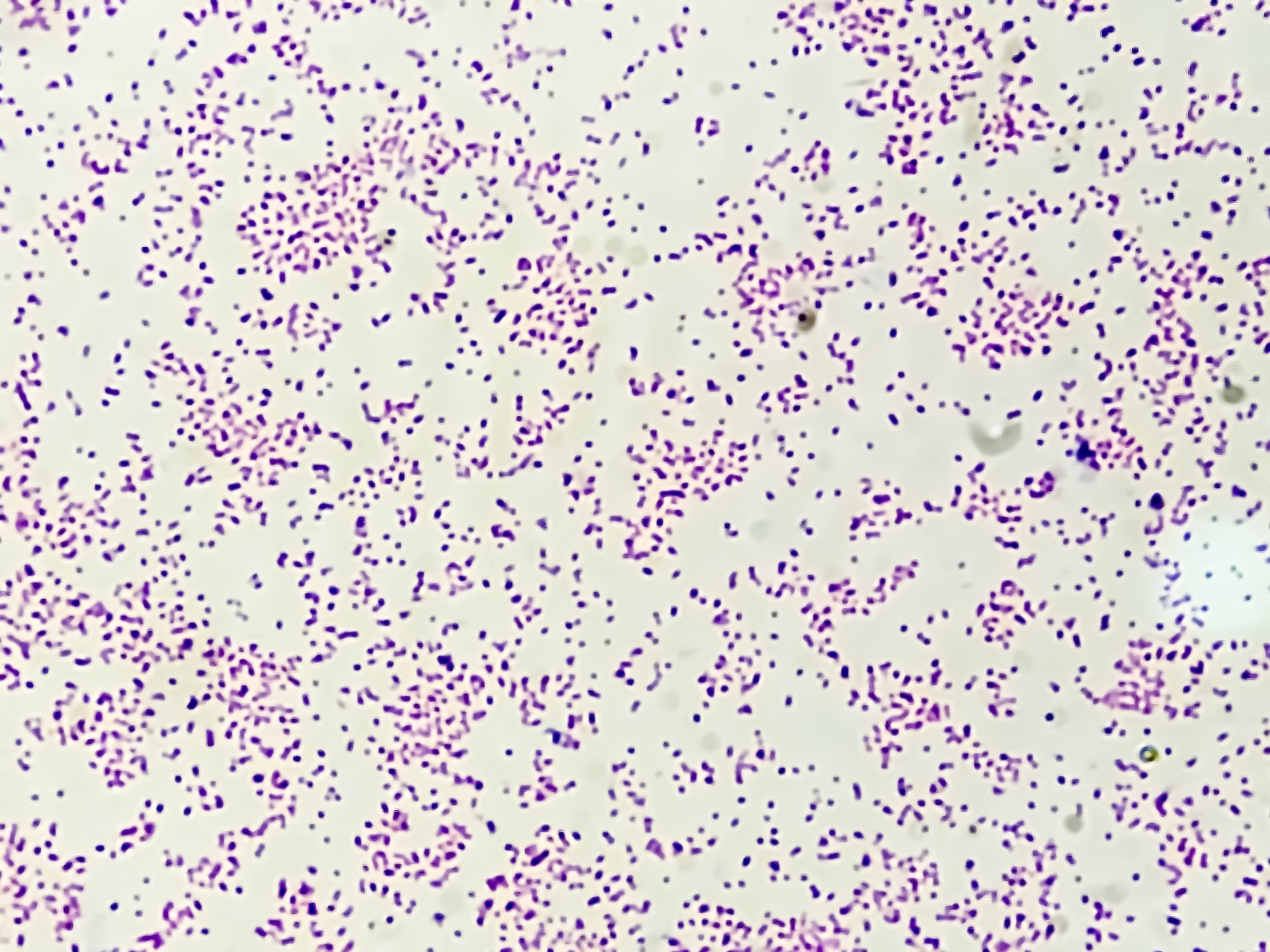
S. epidermidis, a Coagulase-Negative Staphylococci (CoNS) family member, is widely recognized as the CoNS species most commonly linked to clinically manifested infections.
Due to these infections, there has been a notable rise in the number of individuals with compromised immune systems and the utilization of artificial medical devices.
Consequently, these factors have emerged as noteworthy contributors to nosocomial bloodstream infections.
Numerous CoNS nosocomial isolates have shown resistance to methicillin and other frequently used antibiotics. Due to their remarkable efficacy, glycopeptide antibiotics such as vancomycin and teicoplanin were employed in treating CoNS infections.
However, in recent years, the number of S. epidermidis strains having minimal inhibitory concentrations (MICs) = 8 or ≥ 16 mg/L has increased.
Due to the scarcity of other antibiotics, infections caused by Teico-NS S. epidermidis are becoming a more significant clinical issue. The regulatory pathways underlying teicoplanin resistance are still unknown, and there is a lack of information on epidemiological studies of Teico-NS CoNS.
The present study aimed to elucidate the clinical significance of Teico-NS S. epidermidis by presenting information on patterns in its occurrence over the past six years.
About the study
In this study, an extensive analysis was conducted at Seoul Medical Center, South Korea, to assess all S. epidermidis isolates from January 2016 to December 2021.
Researchers exempted patients with multiple infections, non-hospitalized patients, strains cultured within two days of patient enrollment, strains cultured frequently within three months, no susceptibility results, patients less than 18 years, and patients where culture test results changed.
The study evaluated baseline traits, measured glycopeptide MICs, and looked at the potential link between the yearly usage of teicoplanin and the occurrence of S. epidermidis strains with increased teicoplanin MICs. The authors comprehensively analyzed microbiological, clinical, and demographic aspects obtained from medical records.
All isolates of strains were identified using the advanced MicroScan system in combination with a matrix-assisted laser desorption ionization-time of flight mass spectrometry system. The VITEK 2 and Microscan systems were utilized to conduct antimicrobial susceptibility tests.
The Clinical and Laboratory Standards Institute (CLSI) criteria were used to interpret susceptibility categories. S. epidermidis teicoplanin MIC values were divided into susceptible (< 16 mg/L), non-susceptible (≥ 16 mg/L), and resistant (≥ 32 mg/L) groups. S. epidermidis vancomycin MIC values were classified as either susceptible (< 8 mg/L) or resistant (≥ 8 mg/L).
The age and MIC data were analyzed using the interquartile range and the median tests. Fisher's exact test and the chi-square test were used for comparison between groups; P values under 0.05 were regarded as statistically significant. Data were expressed using frequencies or percentages, and statistical analysis was conducted using SPSS version 26.0.
This research protocol received approval from the Institutional Review Board (IRB) of Seoul medical center in 2022, ensuring adherence to ethical guidelines. The center granted a waiver for informed consent about this retrospective study and the research followed the principles outlined in the Declaration of Helsinki.
Results
During the research timeframe, 787 strains of S. epidermidis were successfully isolated. Out of these, 328 strains from 323 individuals were selected for analysis. From these strains, 17 (5.2%) were categorized as teicoplanin-susceptible (Teico-S) and 311 (94.8%) were categorized as Teico-NS.
Blood samples constituted the majority of infectious specimens collected, making up 87.2% of the cases. Wound samples, abscesses, cerebrospinal fluid, pleural fluid, ascites, jackson-pratt drains, pleural fluid, and central venous catheter tips were also analyzed.
The study compared the clinical traits of strains in the Teico-NS and Teico-S groups. The Teico-NS group had significantly older patients, higher diabetes mellitus, and a higher coronavirus disease 2019 (COVID-19) infection prevalence.
In total, 40 patients (12.2%) were administered with teicoplanin and 105 (32%) with vancomycin. No significant difference in glycopeptide use was found between the two cohorts.
Earlier research studies speculated that susceptible strains of S. epidermidis lack a 39-kDa protein, which is present in the membrane of a resistant strain.
Teicoplanin resistance in specific patients may be associated with prior glycopeptide use, but no difference was observed between the Teico-S and Teico-NS groups in this trial.
The authors postulated that using glycopeptide antibiotics causes antibiotic selection pressure, leading to a decline in Teico-S.
Throughout the analysis from 2016 to 2019, the annual prescription rate of teicoplanin consistently exceeded that of vancomycin. However, its use decreased significantly in 2020.
The findings of this study did not establish a correlation between teicoplanin usage and the emergence of S. epidermidis strains with high teicoplanin MIC values (≥ 16 mg/L). Hence, conducting additional extensive clinical trials encompassing various CoNS and S. epidermidis strains is imperative.
Limitations and conclusion
This investigation is limited as it uses retrospective data from a single healthcare facility, the analysis of only S. epidermidis strains, the exclusion of other CoNS strains, and minimal information on antibiotic usage.
More investigation is required to pinpoint the precise reason for teicoplanin resistance in CoNS.
In conclusion, S. epidermidis strains with elevated teicoplanin MIC values have increased over the six years. The authors highly recommend incorporating a well-established antibiotic management program into clinical practice, in order to encourage the responsible use of antibiotics.
- Kim S, Choi J-P, Oh DH, et al. (2023). Increased incidence of teicoplanin-non-susceptible Staphylococcus epidermidis strains: a 6-year retrospective study. Scientific Reports, 13:12582. doi: 10.1038/s41598-023-39666-6. https://www.nature.com/articles/s41598-023-39666-6
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antibiotic, Ascites, Blood, Catheter, Coronavirus, covid-19, Diabetes, Diabetes Mellitus, Efficacy, Healthcare, Laboratory, Mass Spectrometry, Medical Devices, Membrane, Protein, Research, Spectrometry, Wound

Written by
Susha Cheriyedath
Susha has a Bachelor of Science (B.Sc.) degree in Chemistry and Master of Science (M.Sc) degree in Biochemistry from the University of Calicut, India. She always had a keen interest in medical and health science. As part of her masters degree, she specialized in Biochemistry, with an emphasis on Microbiology, Physiology, Biotechnology, and Nutrition. In her spare time, she loves to cook up a storm in the kitchen with her super-messy baking experiments.





