Skip to:
- Antihistamines
- Sedating antihistamines
- Central side effects
- Anticholinergic and alpha-adrenergic side effects
- Cardiac side effects
- Side effects with geriatric use
- Contraindications to sedating antihistamines
- Non-sedating antihistamines
- Conclusion
Allergies have gone up by 40% in recent years, and allergy medications are being used more often than ever before. There are various types of allergy drugs. Some are used to control acute attacks whereas others help prevent or alleviate the severity of allergic reactions. Some of them, especially sedating antihistamines and corticosteroids, are known to produce unwanted effects that limit their use in certain conditions.

Antihistamines
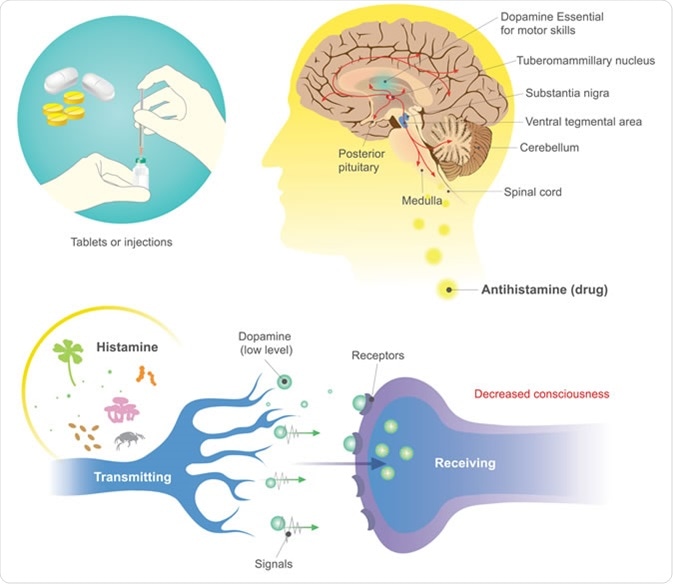
Antihistamines act to prevent the action of histamine, a bioactive amine, at one of the histamine receptor, to block itching, swelling, redness, nasal congestion, teary eyes, cough, nausea and dizziness.
Histamine affects smooth muscle and blood vessels, causing smooth muscle spasm and vasodilation. The administration of antihistamines blocks most of these effects, making them the most commonly used drugs in the world.
These medications come in handy for a variety of allergic conditions as well as those associated with wakefulness and anxiety. Thus, in addition to treating allergies, they have been used variously to treat cold symptoms, motion sickness, nausea due to other causes, skin allergies, and to induce sleepiness in tense or anxious patients.
Antihistamines may be classified as sedating (first-generation antihistamines), and non-sedating (second-generation antihistamines). Both act on the H1 receptor, but the first-generation drugs act less selectively on other receptors as well. The difference lies in their ability to cross the blood-brain barrier.
Sedating antihistamines
These drugs have a common chemical structure with drugs which antagonize muscarinic receptors and cholinergic receptors; some antihypertensive drugs; and some tranquilizers. They are not selective to histamine receptors, as a result. They have anti-muscarinic effects, anti-alpha-adrenergic effects, and anti-serotonin effects.
Sedating antihistamines easily cross the blood-brain barrier, to act on central histamine receptors as well as those located peripherally. There are about 64,000 neurons in the human brain which secrete histamine. These regulate a host of actions, namely:
- Wakefulness
- Learning and memory
- Anti-appetite
- Regulation of body temperature
- Regulation of heart rate and blood pressure
- Involvement in stress hormone and endorphin release
Central side effects
Since these actions are disrupted by sedating antihistamines, these drugs produce sedation, drowsiness, tiredness, lack of concentration, difficulty in learning and memory tasks, poor examination performance, and difficulty with work or driving due to cognitive and coordination problems. Moreover, users continue to feel tired, inattentive, forgetful, and experience poor motor and sensory performance the morning after a night dose – mostly because histamine reduces the duration of rapid eye movement (REM) sleep.
Anticholinergic and alpha-adrenergic side effects
Moreover, sedating antihistamines also produce effects via their blockade of the cholinergic and alpha-adrenergic receptors, such as urinary retention, constipation, sinus tachycardia, inhibition of bowel motility, agitation, and worsening of narrow-angle glaucoma. They also produce or worsen dryness of the mouth, increase the appetite, and induce tolerance when used beyond 5 days or so.
Blurred vision, pupillary dilation, dryness of the mouth and skin, flushing, delirium and confusion, and hyperthermia comprise the well-known and life-endangering anticholinergic syndrome caused by high doses of these drugs. Many over-the-counter antihistamines contain a decongestant as well, and therefore if the user experiences palpitations, the medication should be stopped.
Cardiac side effects
Astemizole and terfenadine are two H1-antihistamines which prolong the cardiac QT interval, and can produce dangerous irregularities of the heart rhythm such as the characteristic 'torsades des pointes' in the ventricular myocardium. These are not approved for use in most countries currently, as a result. This issue is also seen with large doses or overdoses of certain sedating antihistamines like brompheniramine, promethazine, or diphenhydramine.
Side effects with geriatric use
These drugs should be used cautiously in older patients because they typically have lower numbers of cholinergic neurons in the brain, have fewer cholinergic receptors, have compromised renal and liver function, and a less stable blood-brain barrier, with increasing age. Even at lower doses, they can produce dizziness, lowering of blood pressure, and sedation carrying over to the next day. This can cause older adults to fall with related injury risks.
About 25% of older people (over 65 years) have some cognitive decline, even if this is subtle or unnoticed. These individuals may respond badly to antihistamines with pronounced anticholinergic effects, and may show signs of dementia as a result.
Delirium or impaired cognition are other associated side effects with the use of sedating antihistamines in older people. This may further result in inappropriate treatment with antipsychotics, and committal to long-term care facilities with hallucinations and other signs of agitation or aggression, caused by the anticholinergic drugs.
Doctors and other healthcare professionals, as well as older patients, should avoid these drugs now that non-sedating antihistamines are available.
Contraindications to sedating antihistamines
These drugs should be avoided in very young children and in conditions like:
- urinary retention due to benign prostatic hyperplasia
- closed-angle glaucoma
- cardiac disease
They should be used with caution and only if essential, in patients with:
- pregnancy
- constipation
- xerostomia or dryness of the mouth
- hyperthyroidism
- asthma
- chronic obstructive lung disease
- renal disease
- liver disease
- benign prostatic hyperplasia, which is associated with chronic urinary retention
- patients on antidepressants or seizure medication should also consult their doctors before taking antihistamines
- In patients who drink alcohol
With the availability of second-generation antihistamines, the older sedating antihistamines should be avoided if possible. In any case, individuals who are about to write examinations, who are learning exacting materials or tasks, and adults who must fly, drive or work at any task requiring focused concentration should avoid using these drugs.
Non-sedating antihistamines
These are also called second-generation H1-antihistamines, and include loratadine, fexofenadine, mizolastine, ebastine, azelastine, cetirizine, desloratadine, and levocetirizine. These have no currently known cardiac side effects.
Sedation
Fexofenadine and desloratidine, which, along with levocetirizine, are the most commonly used non-sedating antihistamines, cause very little sedation, as they do not cross the blood-brain barrier to any significant extent and thus have little effect on histamine receptors in the brain. Their failure to cause central sedation is due to their interaction with a pump protein, P-glycoprotein, which inhibits their translocation across the blood-brain barrier. Levocetirizine may produce sedation in a percentage of patients, though it needs to be taken at higher than recommended doses for this.
With their freedom from off-target effects, the non-sedating antihistamines are much more suitable for patients who need long-term therapy. Not only are they safer, but they have a more potent anti-allergic effect.
Liver injury
Non-sedating antihistamines can rarely cause acute liver injury. Although the liver damage is typically mild, if it occurs, antihistamines should be stopped. The liver function is usually only slightly deranged, and returns to normal with substitution of another antihistamine or cessation of the therapy. Thankfully, stopping these drugs produces prompt reversal of most of these side effects, which are typically mild.
Conclusion
The newer antihistamines are generally safe, but should be avoided in children and in pregnancy unless essential.
Sources
- Pharmacology of antihistamines. Martin K. Church and Diana S. Church. Indian Journal of Dermatology. 2013 May-Jun; 58(3): 219–224. doi: 10.4103/0019-5154.110832. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3667286/
- Coggins, Mark D. Antihistamine risks. Today’s Geriatric Medicine. https://www.todaysgeriatricmedicine.com/archive/0313p6.shtml
- Livertox.nih.gov. (2019). Cetirizine and levocetirizine. https://livertox.nih.gov/Cetirizine_Levocetirizine.htm
- Livertox.nih.gov. (2019). Antihistamines. https://livertox.nih.gov/Antihistamines.htm
- Mayoclinic.org. Allergy medications: know your options. www.mayoclinic.org/…/art-20047403
- Smith N., et al., (2015). Long-term antihistamine therapy revisited. SA Pharmaceutical Journal. https://www.researchgate.net/publication/283758657
- Drugoffice.gov.hk. (2012). Oral anti-allergy medicines. www.drugoffice.gov.hk/…/dm_08.html#e
- Simsek A. et al., (2016). The effect of long-term use of intranasal steroids on intraocular pressure. Clinical Ophthalmology. https://dx.doi.org/10.2147%2FOPTH.S106392.
Further Reading
- All Allergy Content
- What are Allergies?
- Different Types of Allergies
- Old Friends Hypothesis
- What is the Microbial Diversity Hypothesis?
Last Updated: Nov 15, 2019

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article






