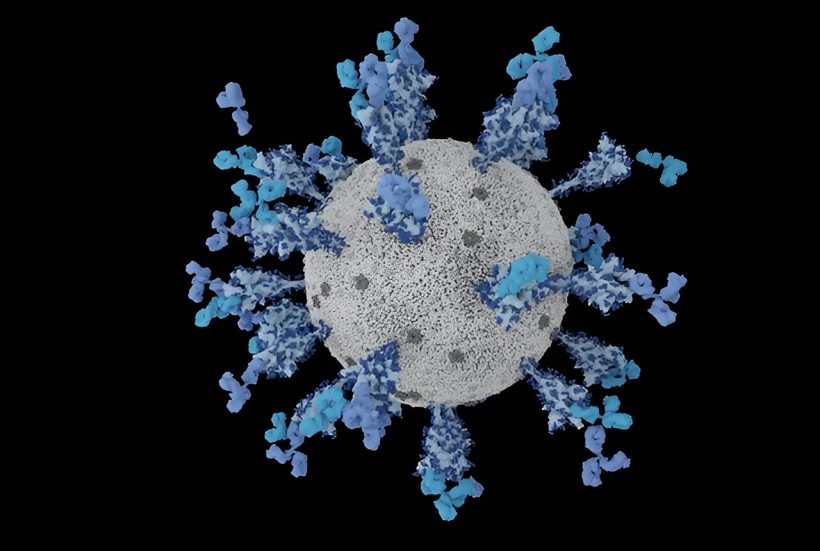
The omicron variants of the SARS-CoV-2 virus, which have rapidly spread around the world over the past year, latch onto our cells more tightly, invade them more efficiently, and elude many of the antibodies induced by previous infections and vaccines. These are some of the key findings from a multinational team of researchers reporting today in the journal Nature.
The lead authors of the study were Amin Addetia, a graduate student, and Young-Jun Park, a research scientist, in the laboratory of David Veesler, professor of biochemistry at the University of Washington School of Medicine, and Luca Picolli, director of Humabs BioMed, Bellinzona, Switzerland, and James Brett Case of the Washington University School of Medicine in St. Louis. Veesler, who is also a Howard Hughes Medical Institute Investigator, headed the study.
“The omicron variants that have become dominant over the past year, such as BQ.11 and XBB.1.5, have high affinity for the receptor on host cells, angiotensin-converting enzyme 2, and they are able to fuse with the cell membrane and invade much more efficiently than previous SARS-CoV-2 omicron variants,” Veesler said.
Since the 2019 outbreak of SARS-CoV-2 in Wuhan, China, the virus has continually evolved. New variants of the original strain are constantly emerging. In some cases, these variants have proved to be less fit, thereby limiting their spread. But in other cases, more efficient variants have caused waves of infections and deaths.
The first omicron variant, designated BA.1 has been followed by a series of variants, each with mutations that increased their ability to infect and spread. These include variants designated BA.2, BA.4, BA.5, BQ.1.1, XBB and its derivatives XBB.1 and XBB.1.5.
They have also been able to reinfect people who had been infected by earlier variants and break through the immune protection of vaccines designed to protect against the earlier variants. These reinfections and breakthrough infections are possible because the new variants can evade antibodies induced by exposure to the earlier variants, Veesler and his colleagues found. Such antibodies, called neutralizing antibodies, prevent infection by quickly clearing an invading virus before it can become established.
However, the researchers also found that previous infection or vaccination did help to generate antibodies that recognized some of the proteins found on newer variants. These antibodies successfully activate immune cells that eradicate infection by killing and eliminating infected cells.
This immune response may explain why previous exposure to earlier variants or vaccination against them appears to reduce the risk of serious illness, hospitalization, and death with reinfection by a newer variant, Veesler said.
Although the neutralizing activity of most antibodies generated against earlier variants was much reduced, the effectiveness of one antibody, called S309, was retained.
This antibody targets a region on the virus’ spike protein that tends to remain relatively unchanged from variant to variant, presumably because its role is essential for the virus to function.
“S309 still recognizes all these variants and neutralizes them (albeit less efficiently), promotes the cellular response, and protects against disease in animal studies,” Veesler said.
The scientists explained one reason why previous infection or vaccination against earlier variants does not protect against infection by new variants as efficiently as with earlier variants: The immune system tends to react by producing antibodies induced by previous variants and cross-reacting with newer variants instead of producing new bespoke antibodies tailored to target the altered proteins on the new variants.
Veesler suspects this is due to a phenomenon called immune imprinting in which the immune response to a new infection by a similar virus is heavily influenced by the immune system’s earlier response. This immune imprinting leads it to concentrate on what it knows instead of learning new tricks to tackle the mutations found in the new variant.
This phenomenon is one reason why vaccines against new variants should not contain components from older variants that might favor immune imprinting and lead to a less effective immune response, Veesler said.
More information:
Amin Addetia et al, Neutralization, effector function and immune imprinting of Omicron variants, Nature (2023). DOI: 10.1038/s41586-023-06487-6
Journal information:
Nature
Source: Read Full Article