In a new study, researchers at the University of Oregon’s Phil and Penny Knight Campus for Accelerating Scientific Impact used start codon disruption with CRISPR-Cas9 gene editing to prevent Fuchs’ corneal dystrophy in mice. It is the first demonstrated use of the technique, called start codon disruption, to treat a genetic disorder in post-mitotic tissue, and has potential to revolutionize treatment of Fuchs’ dystrophy by replacing the need for corneal transplant. It could also lead to new treatments for other genetic diseases, even disorders affecting non-reproducing cells.
The new paper, “Start codon disruption with CRISPR/Cas9 prevents murine Fuchs’ endothelial corneal dystrophy,” was led by Knight Campus research professor Balamurali Ambati and published in the journal eLife.
The paper details the results of an 8-year study that addresses a disease affecting roughly one in 2,000 people globally. Fuchs’ corneal dystrophy causes corneal endothelial cells to die off, causing swelling that can lead to decreased vision, pain, visual impairment and blindness.
“There’s lots of people working on trying to keep these cells from dying but the challenge, ultimately, is that these are post-mitotic cells—you are born with the cells that you’re going to have and when they start dying off that becomes a problem,” Ambati said.
Currently the only treatment for Fuchs’ dystrophy is corneal transplant, a major surgery with associated risks and numerous potential complications, such as infection, rejection and glaucoma. The disease is the leading cause of corneal transplant in the U.S., and although corneal tissue is readily available in this country., it is in short supply throughout much of the world.
Investigators focused on an early-onset subset of the disease that typically strikes patients in their late 30s or early 40s. They zeroed in on a single-point mutation in a collagen protein known as COL8A2, or collagen type VIII alpha 2 chain.
“What was previously demonstrated was that if you knock out this gene (COL8A2), the corneas are fine,” Ambati said. “It’s specifically this mutant form of this protein that’s causing the problem.”
Researchers sought to test whether knockdown of the protein could offer a new therapeutic strategy for the disease. They turned to CRISPR-Cas9 gene editing to target the pathogenic protein in adult mutant mice, but faced the challenge of using the technology on post-mitotic cells.
“With a post-mitotic cell, it’s very difficult or impossible to induce homologous recombination. Therefore, we have to think of other ways to accomplish our goal.” said Hironori Uehara, a researcher in Ambati’s lab and a lead author on the paper.
Uehara developed an innovative means of blocking the expression of the COL8A2 gene by targeting its start codon. The start codon is the initiation site of protein synthesis. Disruption of the start codon can result in termination of the protein expression. Targeting other sites can also terminate the protein expression by frame shift, but it may induce other unwanted protein expression. The farther one targets downstream from the start codon, the greater the risk of missense mutations that result in viable mutant proteins with unknown activity.
“We determined that we could disrupt the start codon and thereby knock down that protein expression selectively by delivering that gene therapy just to the cornea,” Ambati said.
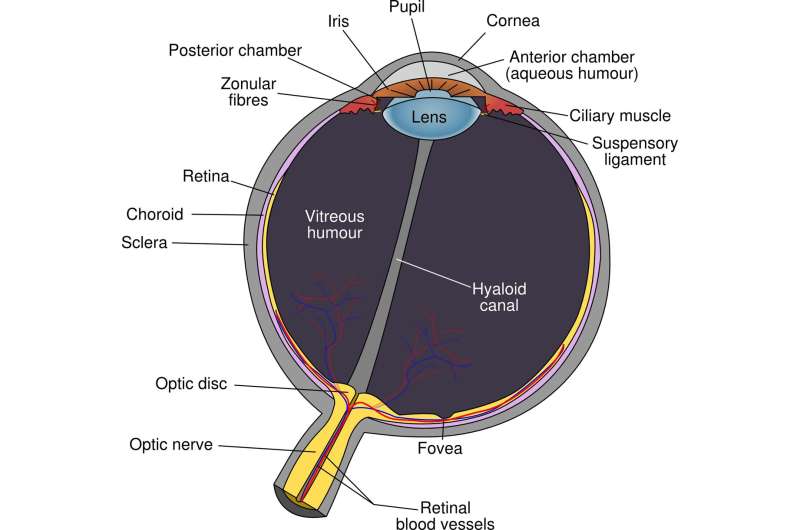
The research team delivered the treatment via adenovirus encoding SpCas9 and guide RNA by injection into the anterior chamber of the mouse eye, which directly faces the corneal endothelial cells. In studies examining the safety of the treatment, they determined that the surrounding tissues were not affected by the gene therapy. They studied other off-target genes to make sure they had not been affected and determined the maximum tolerated dose was safe for the retina, iris and other parts of the eye.
The research team showed they could not only preserve the density and structure of the endothelial cells in the cornea, but also that they could rescue their function. During functional rescue tests in which swelling was induced, they made some surprising secondary discoveries about the cornea. Applying water to the cornea did not induce swelling as researchers expected. Instead, they determined that swelling was induced by ingress of aqueous humor into the cornea through the corneal endothelium (the back side of the cornea), and hence that hyperosmolar solution challenge on the surface of the cornea after epithelial removal resulted in the most corneal swelling.
The research team used mice bred by Dr. Albert Jun at Wilmer Eye Institute at Johns Hopkins University, in Baltimore, MD, with a mutation identical to the one responsible for Fuchs’ dystrophy in humans. Jun was a contributing author on the paper.
The study lays the groundwork for future research examining the viability of using COL8A2 gene knockdown as a therapeutic for Fuchs’ dystrophy in animals, non-human primates and eventually in clinical testing involving humans. Reducing the need for corneal transplants for Fuchs’ dystrophy patients could indirectly help other patients in need of corneal tissue, Ambati said. Future studies could also explore the impact of Cas9-mediated gene knockdown to target other genetic disorders in post-mitotic cells with a single-point mutation, including neurologic diseases, immune diseases and certain disorders affecting the joints.
Source: Read Full Article






