A new study has found substantial regional differences in access to transcatheter aortic valve replacement (TAVR) and patient outcomes between Ontario and New York State. New York residents had improved access to TAVR and improved outcomes compared to Ontario. Statistical modeling also indicated that the same New York residents would have had worse outcomes had they been treated in Ontario. Results are published in the Canadian Journal of Cardiology.
TAVR has revolutionized options for treating patients with symptomatic severe aortic stenosis, one of the most common and serious types of heart valve disease and has become the standard of care for a wide spectrum of patients over the last two decades. Current clinical practice guidelines recommend TAVR as the treatment of choice for patients deemed at prohibitive or high risk for surgical aortic valve replacement (SAVR) and a reasonable alternative for patients at intermediate or low risk. However, there are wide regional variations in access to TAVR.
In many jurisdictions, the demand for TAVR has exceeded capacity, resulting in poor access, with potentially a higher threshold for offering therapy or longer wait times and substantial wait-time morbidity and mortality.
“These potential patient harms must be weighed against the possible benefits of centralizing TAVR procedures to fewer specialized centers with potentially higher procedural volumes,” explained lead investigator Harindra Wijeysundera, MD, Ph.D., FRCPC, Schulich Heart Program, Sunnybrook Health Sciences Centre, University of Toronto, Canada.
“In jurisdictions such as New York, there has been rapid dissemination of new TAVR centers, providing additional capacity, but with relatively low volumes at some institutions. Given the relationship between low operator-hospital volume and poorer outcomes seen in TAVR, this raised concerns of potentially poorer postprocedural outcomes being a possible clinical consequence if the availability of TAVR was more widespread.”
Because little is known about how these two opposing scenarios compare (potentially sicker patients preprocedurally, but with potentially improved postprocedural outcomes given the higher operator-hospital experience, versus less-sick patients with shorter wait times, but potentially poorer postprocedural outcomes because of lower operator-volume experience) investigators developed a study to address this gap in knowledge.
Investigators compared outcomes between Ontario, Canada, and New York State, USA, as a natural experiment comparing two healthcare systems with substantially different capacities to perform TAVR. Their objective was to determine whether differences in healthcare delivery in jurisdictions with high versus low access of care to TAVR translate to differences in postprocedural mortality and readmissions.
In this observational, retrospective cohort study, investigators identified all Ontario and New York State residents over 18 years of age who received TAVR from January 1, 2012, to December 31, 2018. The primary outcomes were post-TAVR 30-day in-hospital mortality and all-cause readmissions.
The investigators found substantial differences in access between the two jurisdictions. In Ontario, with a population of 14.8 million and a surface area of 1,076,395 square kilometers, there were 5,007 TAVR procedures performed at 11 hospitals, with access rates increasing from 18 in 2012 to 87 TAVR per million in 2018.
In New York State, with a population of 19 million and a surface area of 141,300 square kilometers, there were 16,814 TAVR procedures performed at 36 hospitals, with access rates increasing from 32 in 2012 to 220 TAVR per million in 2018. There was no difference in the rate of readmission at 30 days (14.6% in Ontario and 14.1% in New York State), but 30-day in-hospital death was higher in Ontario (3.1%) than in New York State (2.5%).
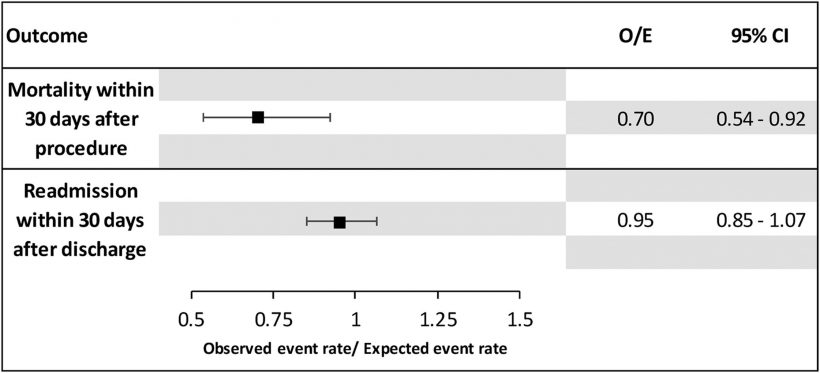
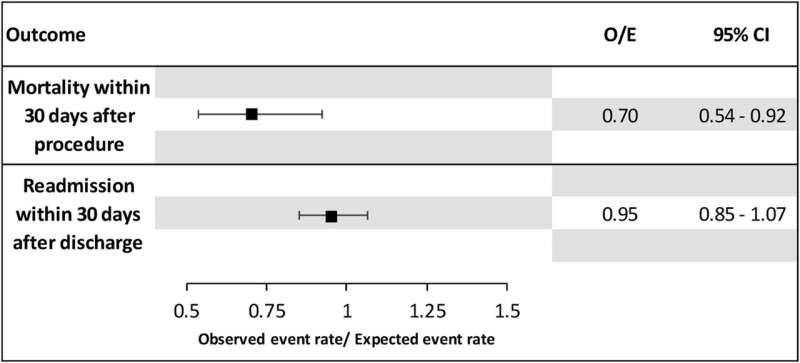
Investigators calculated the observed versus expected outcomes for New York patients had they been treated in Ontario.
“It appears that having greater access to TAVR is associated with improved outcomes, potentially because of intervention earlier in the trajectory of the disease,” commented Dr. Wijeysundera. “This calls for further research to understand the optimal balance between overall TAVR capacity, as well as individual operator and institution volume.”
In an accompanying editorial, Stéphane Noble, MD, Structural Heart Unit, University Hospital of Geneva, Geneva, Switzerland, and colleagues noted that as a direct consequence of the increasing demand for TAVR, procedures are not being matched by the growth in capacity, waiting lists are progressively growing, and this is associated with a risk of death and hospitalization for heart failure while waiting for the procedure.
High-volume centers report better results than low-volume centers, and this is mainly because of their organization and protocols. In addition, low-volume operators perform better at high-volume centers than at low-volume centers. “Indeed, access to timely treatment is as important as having access to high-volume centers with experienced operators who can perform complex procedures,” commented Dr. Noble.
“TAVR remains underperformed in Ontario compared with New York State (three-fold greater access in New York) and western European countries mainly because of funding difficulties and lack of capacities to cover a large territory. Access to timely treatment earlier in the disease process of aortic stenosis could actually be more cost effective and associated with a better quality of life,” concluded Dr. Noble.
More information:
Harindra C. Wijeysundera et al, Regional Differences in Outcomes for Patients Undergoing Transcatheter Aortic Valve Replacement in New York State and Ontario, Canadian Journal of Cardiology (2023). DOI: 10.1016/j.cjca.2023.01.025
Stéphane Noble et al, Geographic Determinants of Outcomes After TAVR: Should We Favour Timely Access to TAVR Rather Than High Volume Per Centre?, Canadian Journal of Cardiology (2023). DOI: 10.1016/j.cjca.2023.03.006
Journal information:
Canadian Journal of Cardiology
Source: Read Full Article