A newly published Burnet Institute study has demonstrated the feasibility and effectiveness of simplified clinical pathways for treatment of hepatitis C (HCV) in Myanmar.
Conducted between January 2019 and August 2020, the study provides endorsement for a ‘one-stop-shop’ model for HCV treatment and care that could be applied more widely in Myanmar and in other low- and middle-income settings globally.
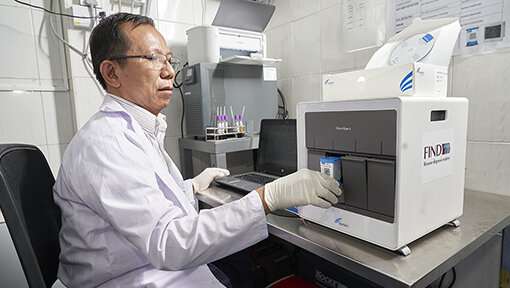
The study was done in partnership with FIND, the global diagnostics alliance as part of the HEAD-Start (Hepatitis Elimination through Access to Diagnostics) portfolio, funded by Unitaid, and published in the journal Liver International.
Lead author, Burnet Research Assistant and Ph.D. candidate Bridget Draper, said the study involved the use of rapid tests, point-of-care GeneXpert diagnostic testing and direct-acting antiviral prescription by general practitioners at decentralized primary care clinics.
The availability of new highly effective pan-genotypic treatments obviates the need for patients to undergo genotyping.
Patients no longer need to visit specialists in hospitals for transient elastography (for example, a FibroScan) for diagnosing cirrhosis as simple blood tests that are widely available used to calculate the APRI score are sufficient.
Ms Draper said the study, involving more than 600 participants from two sites in Yangon—one for people who inject drugs (PWID) run by Burnet Institute Myanmar, and the other for people with liver disease, run by Myanmar Liver Foundation—produced outstanding results with high rates of retention across the cascade of care.
“Almost everyone who started treatment, finished treatment, we didn’t lose anyone before starting treatment,” Ms Draper said.
Ms Draper said the high retention rate of patients in care from the start to finish of treatment is significant.
“The more we lose people throughout the cascade of care, the more expensive it is to get anyone to start treatment, finish treatment, and achieve a cure,” she said.
“Keeping people throughout the care cascade is cost effective, which is important in settings where there are limited resources available to treat and cure people of hepatitis C.
“This study showed that a one-stop-shop model of care led by GPs can provide a really convenient model of care for the patients.”
Ms Draper said she believes most of what was implemented and learned from the study could be easily applied or adapted to other settings.
“We had to get extra equipment, for example, to make sure there was continuous electricity supply at the sites, and ensure stock was stored safely in really high temperatures and humidity, she said.
Study supervisor Professor Margaret Hellard said the study provides an important pathway forward in global efforts to eliminate hepatitis C as a global health threat.
“The vast majority of hepatitis C infections occur in low- and middle-income countries. This work shows that a simple one-stop-shop approach—where testing and treatment occurs in the community—is highly effective,” Professor Hellard said.
The study findings support Myanmar’s national hepatitis C guidelines and the development of formal recommendations from the World Health Organization on simplified service delivery to support the expansion of HCV treatment and testing in other low- and middle-income countries.
HCV is bloodborne and most commonly transmitted through exposure to blood. Infections are usually asymptomatic and a major cause of liver damage and liver cancer.
Source: Read Full Article






