New research to be presented at this year’s European Congress of Clinical Microbiology and Infectious Diseases (ECCMID 2022, Lisbon, 23–26 April) suggests that many of the symptoms connected to post-COVID syndrome (PCC, also known as long COVID) could be linked to the effect of the virus on the vagus nerve—one of the most important multi-functional nerves in the body. The study is by Dr. Gemma Lladós and Dr. Lourdes Mateu, University Hospital Germans Trias i Pujol, Badalona, Spain, and colleagues.
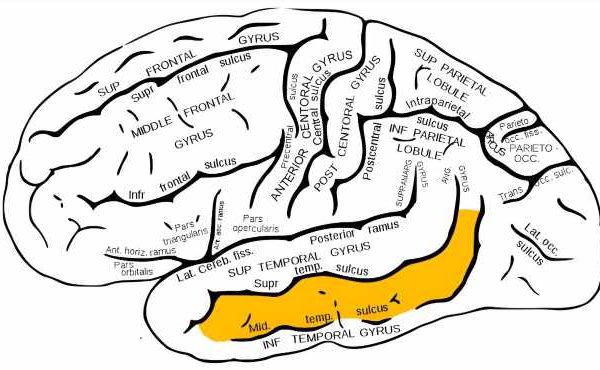
The vagus nerve extends from the brain down into the torso and into the heart, lungs and intestines, as well as several muscles including those involved in swallowing. As such, this nerve is responsible for a wide variety of bodily functions including controlling heart rate, speech, the gag reflex, transferring food from the mouth to the stomach, moving food through the intestines, sweating, and many others.
Long COVID is a potentially disabling syndrome affecting an estimated 10–15 percent of subjects who survive COVID-19. The authors propose that SARS-CoV-2-mediated vagus nerve dysfunction (VND) could explain some long COVID symptoms, including dysphonia (persistent voice problems), dysphagia (difficulty in swallowing), dizziness, tachycardia (abnormally high heart rate), orthostatic hypotension (low blood pressure) and diarrhea.
The authors performed a pilot, extensive morphological and functional evaluation of the vagus nerve, using imaging and functional tests in a prospective observational cohort of long COVID subjects with symptoms suggestive of VND. In their total cohort of 348 patients, 228 (66 percent) had at least one symptom suggestive of VND. The current evaluation was performed in the first 22 subjects with VND symptoms (10 percent of the total) seen in the Long COVID Clinic of University Hospital Germans Trias i Pujol between March and June 2021. The study is ongoing, and continues to recruit patients.
Of the 22 subjects analyzed, 20 (91 percent) were women with a median age of 44 years. The most frequent VND-related symptoms were: diarrhea (73 percent), tachycardia (59 percent), dizziness, dysphagia and dysphonia (45 percent each), and orthostatic hypotension (14 percent). Almost all (19 subjects, 86 percent) had at least three VND-related symptoms. The median prior duration of symptoms was 14 months. Six of 22 patients (27 percent) displayed alteration of the vagus nerve in the neck shown by ultrasound—including both thickening of the nerve and increased ‘echogenicity’ which indicates mild inflammatory reactive changes.
A thoracic ultrasound showed flattened ‘diaphragmatic curves’ in 10 out of 22 (46 percent) subjects (which translates a decrease in diaphragmatic mobility during breathing, or more simply abnormal breathing). A total of 10 of 16 (63 percent) assessed individuals showed reduced maximum inspiration pressures, showing weakness of breathing muscles.
Eating and digestive function was also affected in some patients, with 13 of 18 assessed (72 percent) having a positive screen for self-perceived oropharyngeal dysphagia (trouble swallowing). An assessment of gastric and bowel function performed in 19 patients revealed eight (42 percent) had their ability to deliver food to the stomach (via the esophagus) impaired, with two of these eight (25 percent) reporting difficulty in swallowing. Gastroesophageal reflux (acid reflux) was observed in nine of 19 (47 percent) individuals; with four of these nine (44 percent) again having difficulty delivering food to the stomach and three of these nine (33 percent) with hiatal hernia—which occurs when the upper part of the stomach bulges through the diaphragm into the chest cavity.
A Voice Handicap Index 30 test (a standard way to measure voice function) was abnormal in 8/17 (47 percent) cases, with seven of these eight cases (88 percent) suffering dysphonia.
Source: Read Full Article