More than 50,000 bone marrow-derived stem cell transplants are performed worldwide each year to treat a wide range of conditions, including brain diseases. Before the cells are transplanted, the patients are given chemotherapy to destroy the immune cells and thus prevent the transplanted cells from being rejected by the body. Until now, little was known about the effects of such treatment on the brain. In a new study, researchers from the Paris Brain Institute (Inserm/CNRS/Sorbonne University) and the Institut Pasteur, have looked into this problem. Using an animal model, they discovered how pre-transplant chemotherapy facilitated the replacement of the brain’s innate immune cells, the microglia, by other immune cells derived from the transplanted stem cells (macrophages). These results are published in Nature Medicine.
Many brain diseases lead to progressive demyelination of the central nervous system with devastating neurological symptoms and risk of premature death (e.g. leukodystrophy). Gene therapy aimed at correcting disease-causing genetic mutations directly in bone marrow stem cells, and their subsequent autologous transplantation into patients, has developed in recent years and is now a treatment of choice for many of these conditions.
Clinical studies have shown that the use of chemotherapy prior to bone marrow stem cell transplantation, using a chemotherapeutic agent called busulfan, allows for efficient engraftment and tolerance of the genetically modified cells by the body. However, many questions remain, particularly concerning the mechanisms involved and the impact of this pre-transplant treatment on the patients’ brains.
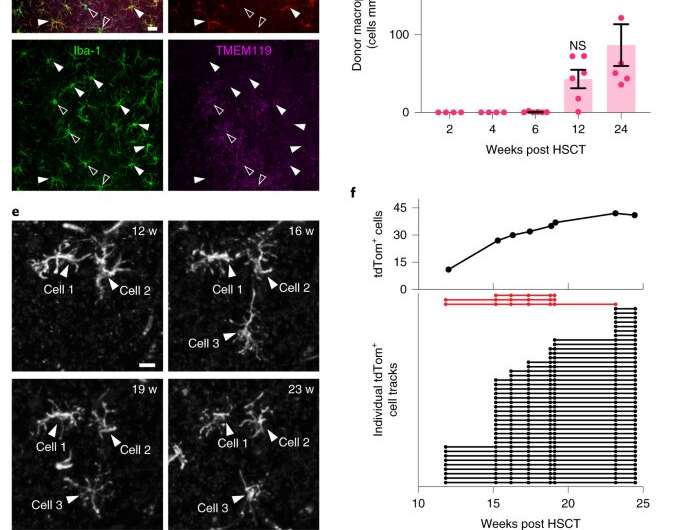
Therefore, the scientists studied the consequences of this treatment on various brain cell populations in an animal model. They looked at microglial cells, brain immune cells that are essential for maintaining healthy brain physiology in normal and pathological states. These cells have a strong capacity for self-renewal throughout life.
In their work, the scientists show that after busulfan chemotherapy, microglial cells completely lose this regenerative capacity, and that many of these cells die by senescence.
However, this process would not be harmful to the brain, since after transplantation, the disappeared cells are quickly replaced by bone marrow-derived cells (macrophages). The microglial cells eliminated by busulfan chemotherapy leave empty niches in the brain that are soon filled by bone marrow-derived macrophages. These macrophages then adopt the morphology and behavior of normal microglia. Future studies will aim to determine whether these macrophages adopt all the properties of endogenous microglial cells in the brain.
“Microglial cells play an essential role in the functioning of the brain and in the pathophysiology of many severe neurological diseases, both genetic and complex, such as multiple sclerosis and Alzheimer’s disease. Understanding the fate of these cells after the transplant process is essential both to clarify the consequences of chemotherapy and to develop new therapeutic strategies for serious neurodegenerative diseases,” explains Nathalie Cartier, Inserm research director in the NeuroGenCell team at the Paris Brain Institute (ICM), and the study’s last co-author.
Source: Read Full Article






