Malaria parasites are rapidly developing resistance to front-line drugs across the world, threatening to undo years of progress in reducing deaths from the disease.
New pictures of a key mediator of drug resistance for the parasite captured with single-particle cryo-electron microscopy by a team of scientists at Columbia University Vagelos College of Physicians and Surgeon—are now giving researchers clues about how to combat resistance.
The study shows that drug resistance in the malaria parasite is linked to a specific protein and illustrates how mutations in the protein allow the parasite to expel the drug.
The new discovery may help scientists find ways to restore the drugs’ potency and will allow health officials in other parts of the world to monitor for emerging resistance.
“The fight against malaria is stalling,” says David Fidock, Ph.D., the C.S. Hamish Young Professor of Microbiology & Immunology, who led the effort with Filippo Mancia, Ph.D., associate professor of physiology & cellular biophysics, and Matthias Quick, Ph.D., associate professor of neurobiology (in psychiatry). “Uncovering the molecular underpinnings of resistance is essential to prolonging the effectiveness of current drugs and developing new ones.”
The research was published Nov. 27 in the journal Nature.
For nearly 15 years, the drug piperaquine, or PPQ, has been used all over the world to treat people infected with the malaria parasite. The drug, in combination with artemisinin, has helped slash the number of deaths caused by the disease from over 1 million in 2004 to an estimated 435,000 in 2017. The disease strikes more than 220 million individuals each year across the globe, including Africa, Southeast Asia, the Western Pacific, and South America. Almost all fatal infections occur in young African children.
But resistance to PPQ has exploded recently in Southeast Asia. “In some areas, the frontline combination of PPQ with dihydroartemisinin (which also has succumbed to resistance) is now effective in only 13% of patients, making this an essentially useless drug in those regions,” Fidock says.
This study in Nature shows that the source of PPQ resistance is a protein in the malaria parasite called PfCRT.
PfCRT is the same protein that had mediated resistance to the former first-line drug, chloroquine (CQ).
That coincidence may create new opportunities for treatment, since the new mutations, which are spreading like wildfire across Southeast Asia, often cause parasites to lose their chloroquine resistance. Combining antimalarials could treat drug-resistant and sensitive parasite infections.
Resistant parasites spit out drug
The antimalarial drugs CQ and PPQ work by entering the parasite’s digestive vacuole (a compartment resembling a stomach) and altering it so that the parasite poisons itself on its own toxic waste product, formed from digested hemoglobin.
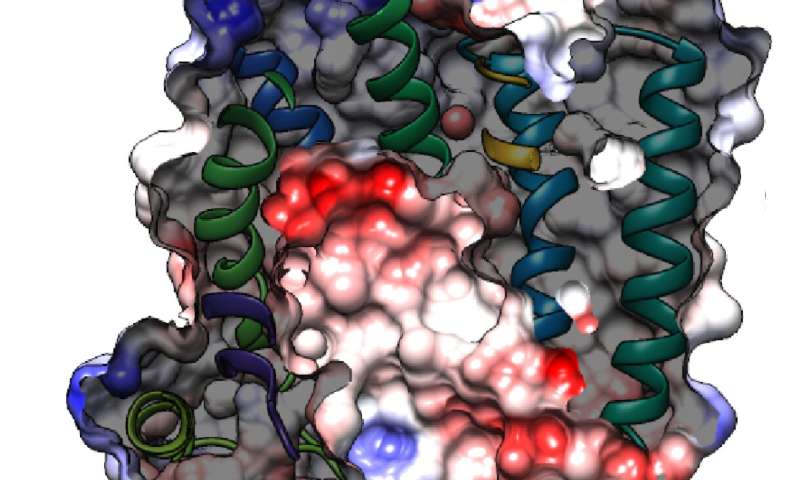
PfCRT is located in the vacuole’s membrane, and the location of mutations—inside a central cavity of PfCRT-reaffirm the observation that resistant parasites use variant forms of this protein to expel the drug out of the vacuole.
“It looked like the protein spits the drug out of the parasite’s stomach,” says Mancia, “keeping it away from its target.”
Though the images were evocative, biochemical testing of the PfCRT’s transport properties was needed to confirm the researchers’ suspicions. By making other mutations in the protein and testing their drug binding and transport abilities, Quick found that only mutations in the protein’s central cavity give PfCRT the ability to expel the drug from the vacuole.
Scientists can now predict how resistance will arise in other parts of the world
With images of PfCRT in hand—combined with the location and properties of resistance-causing mutations—it is now possible to predict how PPQ resistance will arise in other parts of the world.
“The PfCRT gene is difficult to sequence, so it’s been hard for people to monitor,” Fidock says, “There are hundreds of locations in PfCRT that could be mutated, but now we can sayust look at these handful in the central cavity with specific structural and conservation properties. They are the only ones that can drive resistance.”
Based on what’s now known, Fidock says South America could be the next place where PPQ fails. Results presented in this report already show one such mutation in PfCRT that, should it appear and spread in South America, would lead to high-grade resistance and augment the risk of treatment failures.
“Getting ahead of the ‘drug resistance curve’ by knowing where to look in the parasite’s genome will be critical to identifying where resistance arises and having time to move to alternative treatment strategies,” Fidock says.
Fidock and Quick are now testing whether PfCRT mutations identified in Asian malaria parasites will also cause PPQ resistance in African parasites, which are genetically distinct and which cause the vast majority of the global malaria burden. Those experiments may also help officials in Africa who are planning to deploy PPQ more broadly in areas of high transmission and who need to know how to monitor for signs of emerging resistance.
Study suggests ways to restore the potency of antimalarial drugs
Parasites have enlisted PfCRT in their fight against antimalarials, but researchers could also co-opt PfCRT to restore the potency of PPQ and similar drugs.
“We may be able to restore the efficacy of these drugs with an agent that entirely blocks the capacity of this protein to transport anything,” says Fidock, who is working with colleagues to develop parasite-based screens to identify potential candidate compounds.
“That would make PPQ and the earlier first-line drug chloroquine fully functional.”
Limits of Nobel technique pushed to acquire images
The malarial protein (49 kDa) is one of the smallest molecules of its type to be visualized with cryo-electron microscopy (cryo-EM), which is typically limited to proteins of at least 100 kDa in size. PfCRT needed to be bulked up with an antibody fragment before it could be seen under the electron microscope. This fragment, which was found to bind to the PfCRT central cavity, allowed the researchers to see PfCRT from multiple angles, which was necessary to generate a 3-D model.
Source: Read Full Article






