Researchers have boosted pioneering technology to show whether potential treatments are worth progressing into human trials, in a game-changing move that could dramatically reduce the high failure rates in drug discovery and development.
The WEHI-led team is using protein degrader technology to test the efficacy and safety of drugs by better mimicking clinical settings, with a collaborative Australian project already using the system to establish promising drug targets for a range of hard-to-treat cancers.
Almost 95% of biomedical projects fail before entering human clinical trials with the average cost of bringing a new drug to market estimated to be around US$1.8billion. A key issue is the difficulty of assessing a drug’s true safety and effectiveness in preclinical studies.
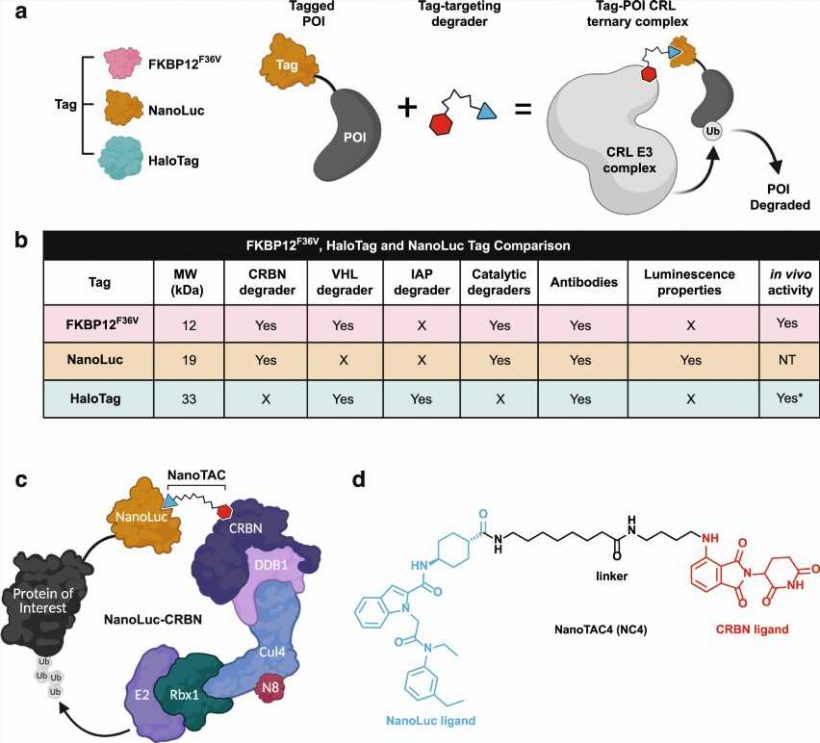
While conventional drug development aims to inhibit the activity of disease-causing proteins, protein degrader technology looks to completely destroy those proteins, with precision targeting.
The technology enables scientists to deliver far more relevant results from pre-clinical testing, to potentially bring safe and effective new treatments to patients faster.
In a new study published in Nature Communications, WEHI researchers Dr. Charlene Magtoto, Dr. Rebecca Feltham and Dr. Christoph Grohmann (now at Nurix Therapeutics) have significantly extended our understanding of one type of protein degrader technology by expanding on current validation strategies, which could boost the number of drugs successfully entering human trials.
A collaboration between WEHI and multiple institutes across Australia is already capitalizing on the revolutionary technology to validate a range of previously “undruggable” proteins and help develop new therapies to treat cancers.
Reimagining drug discovery
About 80% of disease-causing proteins currently cannot be targeted by conventional drugs.
Targeted protein degraders (TPDs), commonly known as Proteolysis targeting chimera (PROTAC), is a pioneering technology that can hit these previously invincible targets.
While current drugs and technology only inhibit the specific activity of a protein, TPDs work by triggering the destruction of the proteins that cause the disease itself.
TPD has the potential to deliver precision treatments by only targeting disease-causing proteins, leaving healthy parts of the body untouched.
The WEHI-led team focused on developing a tag system to help researchers overcome a significant hurdle in the drug development process.
Dr. Charlene Magtoto said this system enables scientists to use drugs that interact with a tag, opening up virtually the entire proteome for target validation.
“Finding a drug to bind onto the protein itself can be difficult and often a reason why researchers reach a crossroads in drug development,” Dr. Magtoto said.
“Attaching a small generic tag onto any protein of interest to enable a destroyer protein to remove it allows us to wipe out any protein just by targeting the tag.
“This is a game-changer technology that will ensure only the best targets enter into drug discovery pipelines.”
Dr. Christoph Grohmann said a partnership with Promega was crucial to developing the new tagging system, collaborating with scientists at the global biotech company and using their NanoLuc luciferase technology.
“WEHI is an emerging leader in TPD technology, and this significant collaboration enabled our team to leverage industrial drug discovery expertise and academic medical research to enhance the technology at a much faster pace,” Dr. Grohmann said.
Crucial cancer targets
The lack of effective new drugs is a particular barrier for cancer researchers, with as few as 1 in 15 developmental drugs progressing into the clinic.
WEHI researchers are working with other institutions across the country to develop TPDs for cancer treatment as part of a current project funded by the Australian Medical Research Future Fund (MRFF).
Dr. Rebecca Feltham, who leads the MRFF tag-degrader program, said the collaboration was helping researchers quickly identify whether their cancer targets were worth pursuing.
“Most of the 150,000 Australians diagnosed with cancer each year are still treated with drugs that came onto the market over 25 years ago, which can cause significant side-effects,” she said.
“As this pioneering technology enables us to better identify genuine targets early in the research process, we could radically accelerate the development of lifesaving new treatments for cancer and other diseases.”
Dr. Feltham has used the tag-targeting TPD technology to investigate 24 potential drug targets—19 of which link to cancer.
Unlike other systems currently used in the field, the protein degradation triggered by tag-targeting TPD technology is reversible. Once the drug is removed, the protein comes back.
“This is exactly what happens in clinical settings and this technology allows us to mimic real TPD treatment scenarios early on in the development process, far better than any technology we have available today,” Dr. Feltham said.
Source: Read Full Article