![Percentage of patients who were persistent with antiobesity medication (AOM) at early stage, medium term, and long term, by AOM agent. [Color figure can be viewed at wileyonlinelibrary.com] Study identifies factors associated with long-term use of FDA-approved anti-obesity medications](https://scx1.b-cdn.net/csz/news/800a/2023/study-identifies-facto.jpg)
A Cleveland Clinic study looked at the long-term use of anti-obesity medications and found that only 19% of the study participants continued to use the medications one year after their initial prescriptions. Participants were more likely to continue to get their prescription filled in the long term if they received more effective anti-obesity medications and experienced more significant weight loss at six months.
The research is published in Obesity Journal.
Hamlet Gasoyan, Ph.D., lead author of the study and a researcher with Cleveland Clinic’s Center for Value-Based Care Research, said, “We now have effective FDA-approved anti-obesity medications. However, this study shows that in a real-world setting, most patients discontinued their prescription fills within the first year. We need to better understand what factors are associated with the decrease in long-term use of those medications.”
Obesity is a common, chronic disease with several causes. According to the Centers for Disease Control and Prevention, the prevalence of obesity is more than 41% among U.S. adults. Obesity increases the risk of major health complications, such as cardiovascular disease and cancer.
A new generation of FDA-approved medications for chronic weight management—such as glucagon-like peptide-1 (GLP-1) receptor agonists—provide effective treatment for obesity. However, there is very limited information on the long-term use of those medications. In addition, studies have shown that discontinuation of treatment leads to weight regain and reduced health benefits.
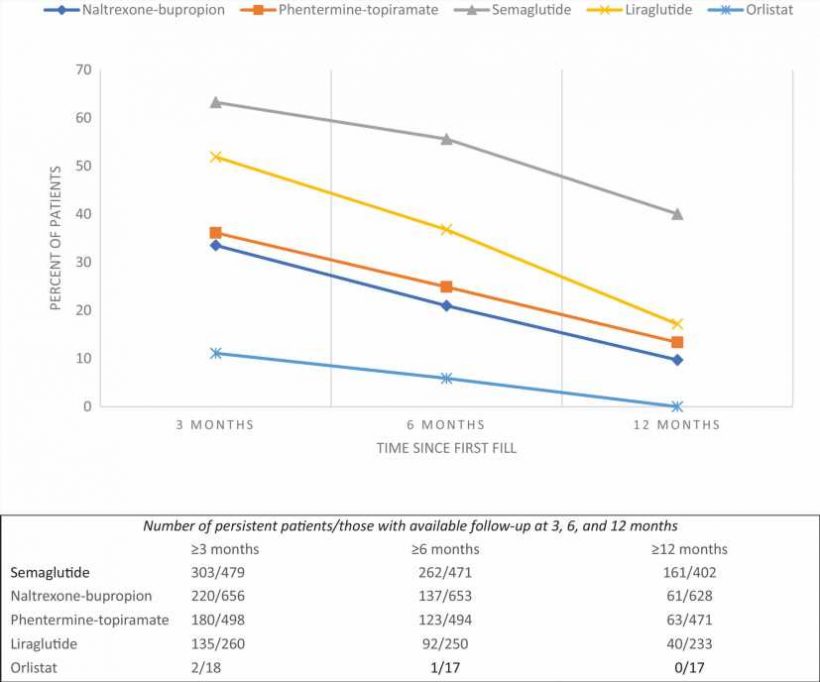
The aim of this Cleveland Clinic study was two-fold. First, researchers examined the continued use of anti-obesity medications at three months, six months, and 12 months. Secondly, the investigators studied the factors associated with continuity of treatment at 12 months.
Study findings showed that 44% of the participants had their anti-obesity medications prescription filled at three months. At six months, 33% of the study participants were persistent with their treatment. At 12 months, only 19% of the study participants continued to get their prescriptions filled.
The Center for Value Based Care Research is part of the Department of Internal Medicine and Geriatrics within the Primary Care Institute at Cleveland Clinic in Cleveland, Ohio.
A total of 1,911 adult participants with a body mass index (BMI) of 30 or greater who had an initial FDA-approved anti-obesity medication filled between 2015 and 2022 were included in this retrospective cohort study. Dr. Gasoyan and colleagues looked at the percentage of participants who persisted with their treatment at 3-, 6-, and 12-months.
Data, including sociodemographic variables, were obtained from the Cleveland Clinic electronic health records (EHR) in Ohio and Florida locations. Anti-obesity medication prescriptions included FDA-approved dosages for chronic weight management, including phentermine-topiramate, naltrexone-bupropion, orlistat, semaglutide injection 2.4 mg, and liraglutide injection 3 mg. Health insurance coverage was classified into private, Medicare, Medicaid, self-pay, and other categories.
To better understand the factors associated with the continued use of anti-obesity medications at one year, researchers looked at the different anti-obesity medications that were prescribed. Among the study participants who received semaglutide, 40 percent of them continued to get their prescriptions filled at one year. In comparison, among the study participants who received an older generation anti-obesity medication, such as naltrexone-bupropion, only 10% continued to get their prescriptions filled at one year.
Another important finding showed that an increase in weight loss at six months is associated with higher odds of long-term use of anti-obesity medications at 12 months.
“While the long-term use of anti-obesity medications remains low, our findings highlight factors that were linked with increased odds of continued treatment. Thus, patients who received more effective anti-obesity medications and those experiencing greater weight loss at six months were more likely to continue to fill their anti-obesity medication prescription at 12 months,” said Dr. Gasoyan.
To further examine what factors may contribute to the long-term use of anti-obesity medications, researchers looked at the health insurance providers of the study participants. The present study’s participants were predominantly privately insured (84%). Researchers found that the insurance carrier (for those who were privately insured) was also a factor when looking at the long-term use of anti-obesity medications. Other determining factors included the medication itself, the percentage of weight loss at six months, and the year when the first prescription was filled.
More information:
Hamlet Gasoyan et al, Early‐ and later‐stage persistence with antiobesity medications: A retrospective cohort study, Obesity (2023). DOI: 10.1002/oby.23952
Journal information:
Obesity
Source: Read Full Article