Throughout the COVID-19 pandemic, using N95 face masks became routine. Researchers at the Shanghai Jiaotong University School of Medicine, China, wanted to know how long durations of mask-wearing might affect health.
In the paper “Evaluation of Mask-Induced Cardiopulmonary Stress,” published in JAMA Network Open , the researchers detail the tightly controlled experiment they designed to evaluate mask-wearing effects on 30 individuals in their late 20s.
To analyze energy expenditure, the study was conducted on one participant at a time in a metabolic chamber, a scientific instrument in the shape of an airtight room. A gas analyzer monitored concentrations of oxygen and carbon dioxide.
Blood pressure, 3-lead ECG heart monitor, and oxygen saturation levels were continuously monitored. Participant physiological activity was monitored with a wearable motion tracking device attached to the right leg during the entire study, except during dual-energy X-ray absorptiometry to measure bone density or while showering.
All participants were fitted with a continuous glucose monitoring sensor and transmitter. Calories of each meal, water intake and physical activity levels were rigorously controlled. Even the urinary nitrogen of the participants was measured.
Each participant spent three days in the chamber, which was furnished with an adjustable bed, desk, chair, exercise bicycle, wash basin, toilet, television and computer. They were allowed to bring their smartphones but were only allowed to use them during sedentary behavior times.
Daily activities during the experiment were strictly controlled according to a standardized schedule that had to be followed by all. Two 30-minute periods of light-intensity exercise were required each day at set times.
Blood samples were obtained before masking, before and after light-intensity exercise, and 14 hours after mask-wearing. Participants were required to rate their overall discomfort using Visual Analog Scales. The questionnaire was administered hourly during the daytime.
All participants were allowed to climatize to the new environment on the first day. On day two, half the subjects wore masks, and the other half did not. Day three reversed the mask-wearing groups so that at the end of the experiment, all participants had spent one day wearing an N95 mask for 14 hours.
The results of this tightly controlled and heavily monitored experiment are unclear as most of the data reported to be collected was not published.
The authors state that wearing the N95 mask reduced respiration rates and oxygen saturation within the first hour they were worn. Because the data was unreported and the results mentioned were unspecified, the significance of the finding is unknown.
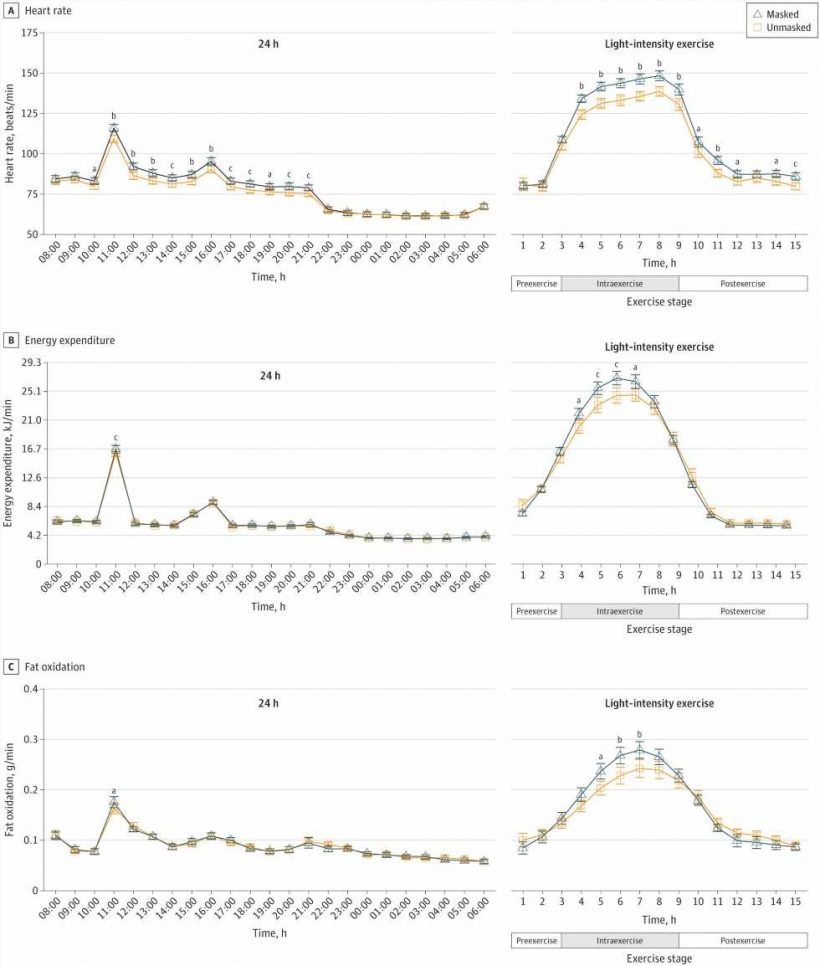
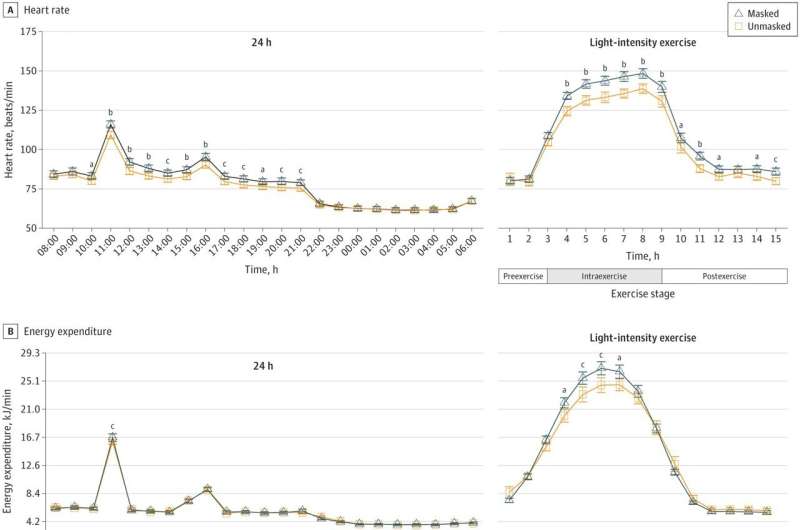
The report on the light-intensity exercise period at 11 am found a mean heart rate of 7.8 beats/min higher, blood pressure slightly higher, energy expenditure and fat oxidation up and respiration rates lower by 4.3 breaths/min.
The fewer breaths with higher energy expenditure and increased heart rates are significant anomalies. It might be plausible if the respiration rate was derived from an aggregate of the metabolic chambers gas analyzer that higher humidity from wearing the mask might have somehow delayed the air exchange, but the reason remains a mystery as the authors make no mention of it.
After the 14-hour mask-wearing phase, venous blood pH decreased, and calculated arterial pH showed a decreasing trend while metanephrine and normetanephrine levels increased. All potentially significant or insignificant results if the data had been included in the paper, but it was not.
The authors conclude that the study demonstrates that wearing the N95 mask for 14 hours significantly affected the physiological, biochemical and perception parameters.
Based on the experimental design, methods detailed, and results stated, nearly all of the collected data is missing from the paper. The study may have demonstrated something, but the published paper does not.
More information:
Riqiang Bao et al, Evaluation of Mask-Induced Cardiopulmonary Stress, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.17023
Journal information:
JAMA Network Open
Source: Read Full Article