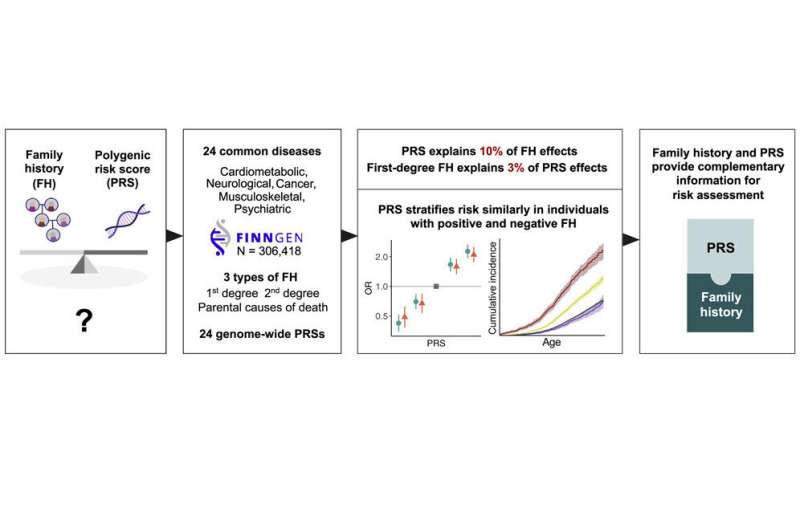
A new study from the University of Helsinki demonstrates the added value of genetic information in measuring inherited disease risk, alongside the widely used assessment of family history.
Physicians widely use family history to assess an individual’s risk of developing common diseases, such as coronary heart disease, diabetes, and cancers. In recent years, polygenic risk scores based on genome-wide DNA testing have been developed for measuring genetic susceptibility. Polygenic risk scores comprehensively measure the individual’s own genetic risk factors.
A study by University of Helsinki researchers has now compared these two measures for more than twenty common diseases. The study looked at diseases such as cardiovascular disease, common cancers and musculoskeletal disorders. The results show that both family history and polygenic risk score measurement provide complementary information for assessment of inherited disease susceptibility.
“Clinicians have asked what polygenic risk assessment adds to the seemingly simple question about family history. Our new results show that the two measures complement each other. Moreover, combining them provides the most accurate information for evaluation of inherited disease risk,” says the study’s first author, Nina Mars, from the Institute for Molecular Medicine Finland (FIMM) at the University of Helsinki.
The study is based on data from the FinnGen research project, with more than 300,000 Finnish biobank participants.
The data showed that the disease risk was particularly high if the individual had both affected family members and a higher-than-average polygenic risk.
The results also reveal that a lower-than-average polygenic risk compensated for the risk-increasing effect of family history. This means that the risk of individuals with a low polygenic risk score was not elevated, even if they had a family history of the disease. The findings were similar across diseases.
Genetic information is more personalized than family history
Although polygenic risk describes an individual’s own genetic susceptibility more accurately than family history, it is not a substitute for family history. According to the research team, there are several reasons for this.
“Family history can, for instance, provide information on non-genetic factors shared by the family, such as lifestyle. However, family history does not provide individualized information. For example, a mother’s illness would lead to similar family history for all siblings, even though each sibling has inherited a unique combination of genetic factors from both biological parents. Polygenic risk assessment measures this unique set of genetic risk factors,” says Nina Mars.
Polygenic risk measurements are currently not widely used in clinical care to assess disease risk.
“Our results complement prior studies that have demonstrated the added value of polygenic risk assessment to existing clinical risk prediction tools. Moreover, polygenic risk information can be assessed simultaneously for a large number of diseases, even for diseases where family history is difficult to survey. And who among us even knows or remembers all our relatives’ diseases?” says Professor Samuli Ripatti from the University of Helsinki, who led the study.
More information:
Nina Mars et al, Systematic comparison of family history and polygenic risk across 24 common diseases, The American Journal of Human Genetics (2022). DOI: 10.1016/j.ajhg.2022.10.009
Journal information:
American Journal of Human Genetics
Source: Read Full Article