A team of international scientists has recently developed virus-like particles (VLPs) by coating liposomes with the synthetic spike (S) glycoprotein of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is the causative pathogen of the coronavirus disease 2019 (COVID-19). In non-human primates, S-containing VLPs exhibit potent immunogenicity characterized by high neutralizing antibody titers and T helper type 1 CD4+ biased T-cell responses.
 Study: Immunization with synthetic SARS-CoV-2 S glycoprotein virus-like particles protects Macaques from infection.
Study: Immunization with synthetic SARS-CoV-2 S glycoprotein virus-like particles protects Macaques from infection.
Background
SARS-CoV-2 is an enveloped ribonucleic acid (RNA) virus that contains S glycoproteins on its surface to assist in its entry into host cells. As the S protein is the most immunogenic viral component of SARS-CoV-2, it is also the primary target of most of the therapeutic monoclonal antibody therapies and vaccines. Importantly, in COVID-19 recovered individuals, an enrichment in S-targeting antibodies has been observed.
In the current study, which is available on the bioRxiv* preprint server, scientists have developed VLPs by coating liposomes with synthetic S trimers and tested their antiviral efficacy in cynomolgus macaques. Cynomolgus macaques are a well-established non-human primate model that is often used to study innate and adaptive immune responses upon infection or vaccination.
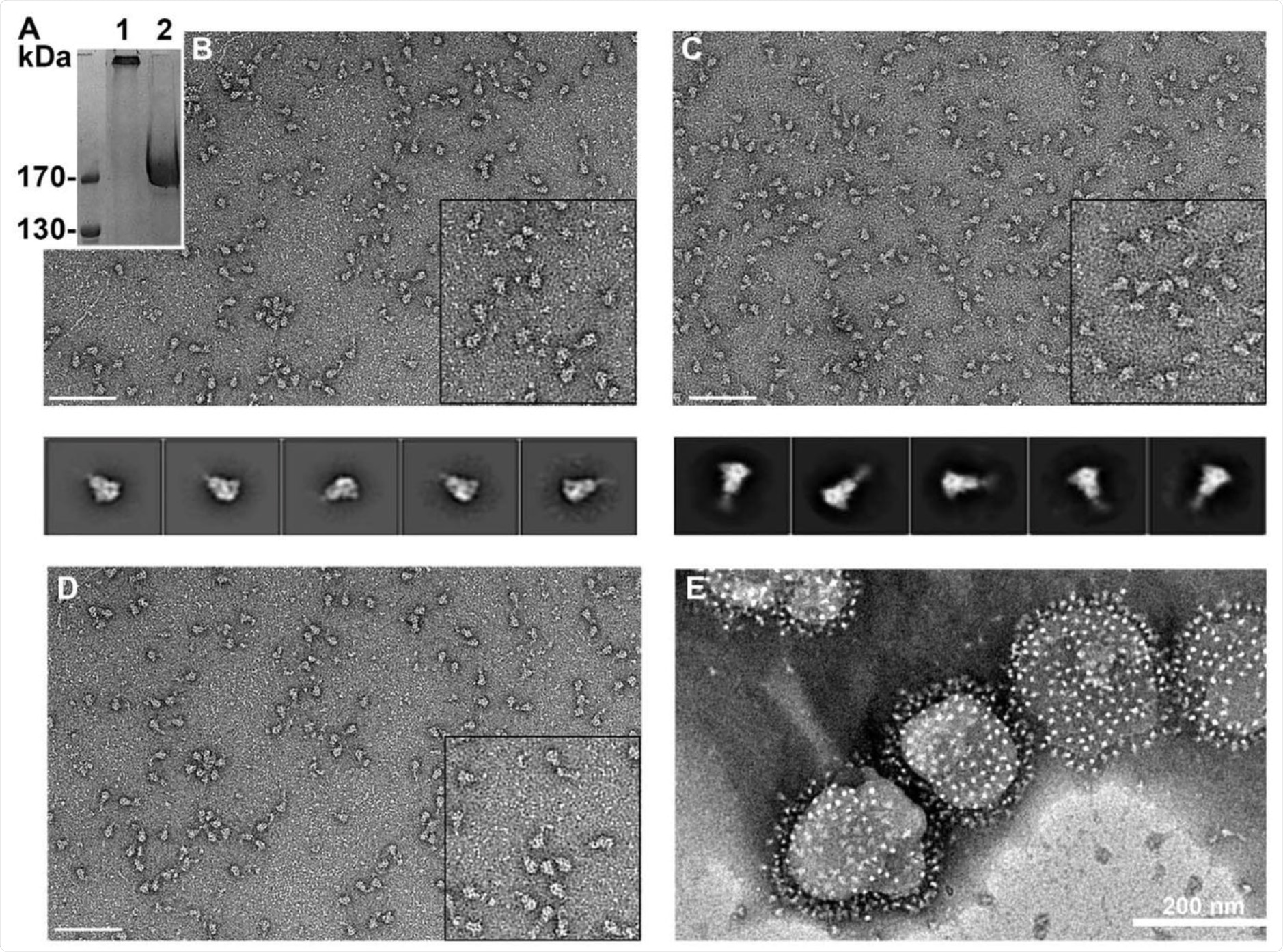
Development of spike-containing VLPs
The scientists produced native S trimers by expressing synthetic S protein constructs in mammalian cells and subsequently purifying them by size exclusion chromatography. Given the low thermostability of the S glycoprotein, the researchers chemically cross-linked S trimers with formaldehyde, which preserved the native structure for a longer time period. The cross-linked S trimers were coated onto liposomes to produce synthetic S-containing VLPs.
Virus neutralizing efficacy of spike-containing VLPs
For safety and immunogenicity profiling studies, the scientists intramuscularly administered cynomolgus macaques with monophospholipid A-adjuvanted S-containing VLPs at weeks 0, 4, 8, and 19. Serum samples were then collected from immunized animals to determine their immunogenic responses.
The study revealed that the 1st and 2nd immunization significantly increased the titers of the anti-receptor-binding domain (RBD)-binding antibodies, whereas the 3rd immunization mainly induced S-specific non-RBD binding antibodies. However, no further induction in antibody titers was observed after 4th immunization.
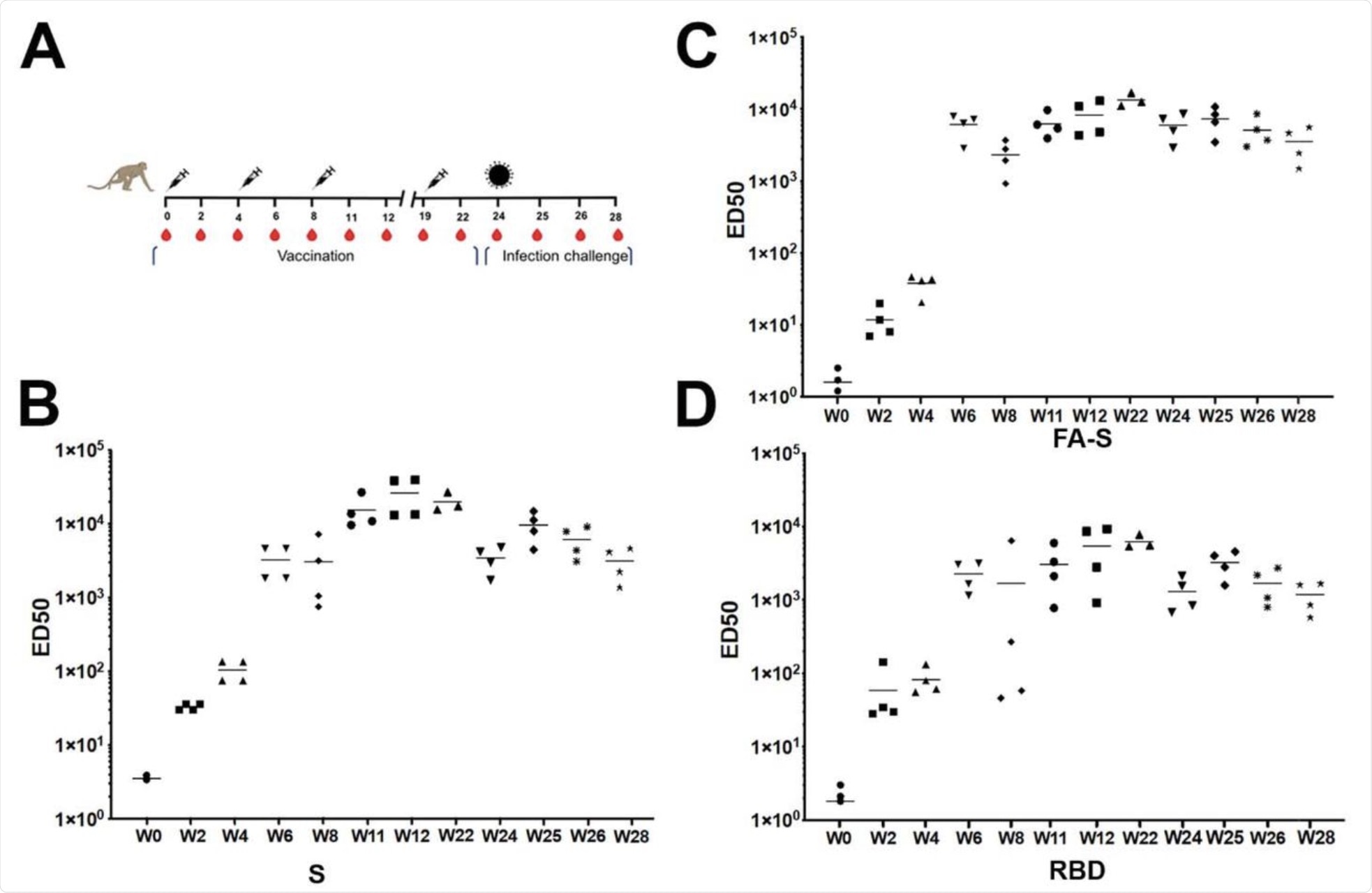 (A) Scheme of vaccination, challenge and sampling. Syringes indicate the time points of vaccination, red drops the time of serum collection and the virus particle the time point of challenge. Symbols of identifying individual macaques are used in all figures. (B) ELISA of SARS-CoV-2 S-protein-specific IgG determined during the study at weeks 0, 2, 4, 6, 8, 11, 12, 19, 22, 24, 25, 28. Median values calculated for the 4 animals are indicated. (C) ELISA of SARS-CoV-2 FA-S-protein-specific IgG determined during the study. (D) ELISA of SARS-CoV-2 S RBD-specific IgG determined during the study.
(A) Scheme of vaccination, challenge and sampling. Syringes indicate the time points of vaccination, red drops the time of serum collection and the virus particle the time point of challenge. Symbols of identifying individual macaques are used in all figures. (B) ELISA of SARS-CoV-2 S-protein-specific IgG determined during the study at weeks 0, 2, 4, 6, 8, 11, 12, 19, 22, 24, 25, 28. Median values calculated for the 4 animals are indicated. (C) ELISA of SARS-CoV-2 FA-S-protein-specific IgG determined during the study. (D) ELISA of SARS-CoV-2 S RBD-specific IgG determined during the study.
The scientists conducted a virus neutralization assay with wild-type pseudovirus, which revealed that the first three immunizations significantly increased neutralizing antibody titers in serum. However, similar to the binding antibody responses, no further boost in neutralizing titer was observed after the 4th immunization.
A similar level of neutralization was also observed against the B.1.1.7, B.1.351, and P1 variants of SARS-CoV-2 after the 3rd immunization with S-containing VLPs. The 2nd immunization appeared to be already sufficient in inducing protective neutralization, as no further increase in titer values was observed after the 4th immunization.
To specifically determine antibody-specific neutralization, the scientists experimentally removed anti-RBD antibodies from immunized serum samples. Interestingly, RBD antibody-depleted sera showed 10 – 30% neutralization. This highlights the neutralizing potency of non-RBD antibodies and the importance of synergy between RBD-specific and non-specific antibodies to achieve high neutralizing efficacy.
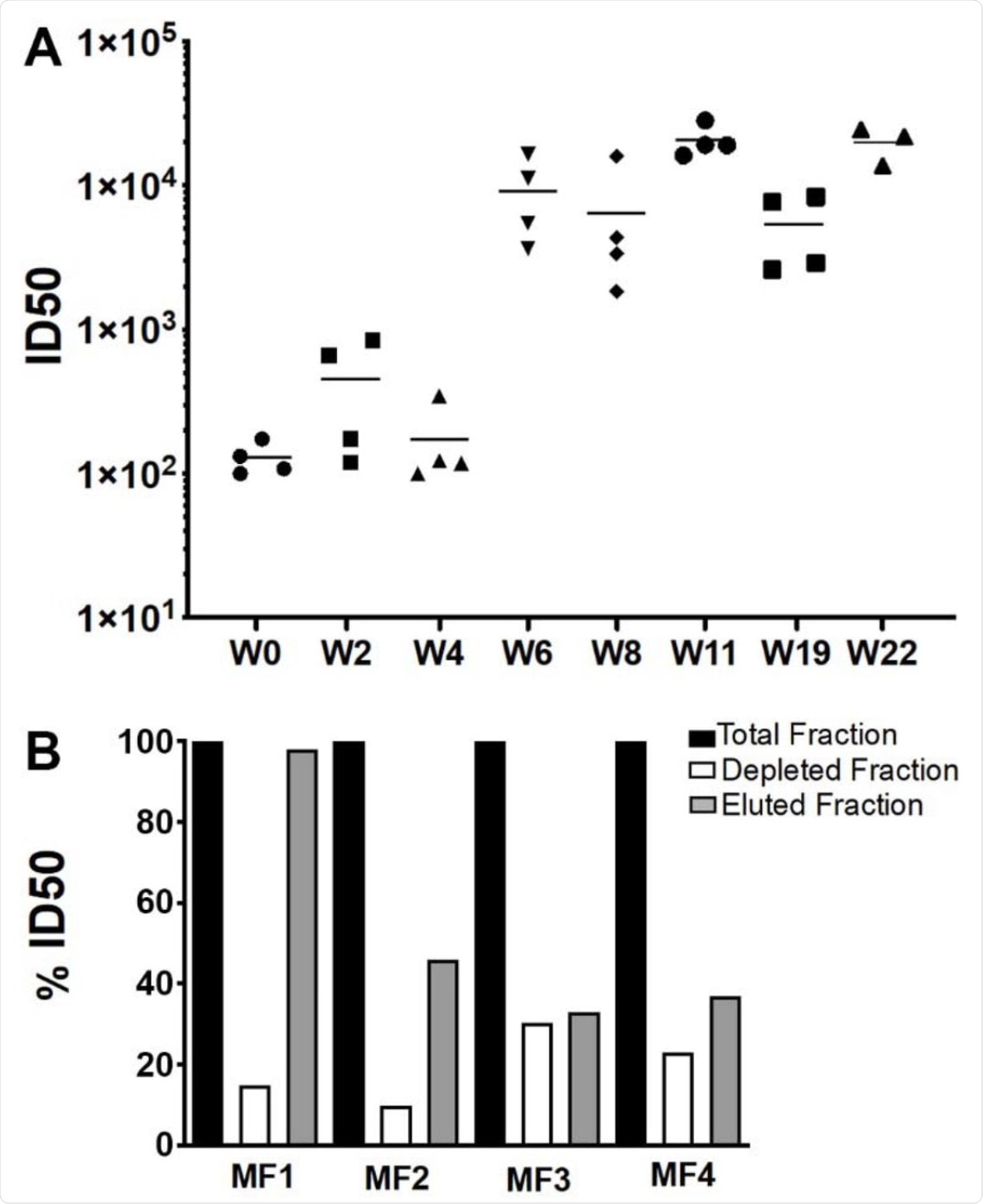 (A) The evolution of SARS-CoV-2 neutralizing Ab titers is shown for sera collected at weeks 0, 2, 4, 6, 8, 11, 12, 19. Bars indicate median titers of the four animals. B) Serum from week 11 was depleted of RBD-specific Abs by affinity chromatography and neutralization activity of the complete serum of each animal was set to 100 % and compared to the RBD-depleted sera and the RBD-specific sera.
(A) The evolution of SARS-CoV-2 neutralizing Ab titers is shown for sera collected at weeks 0, 2, 4, 6, 8, 11, 12, 19. Bars indicate median titers of the four animals. B) Serum from week 11 was depleted of RBD-specific Abs by affinity chromatography and neutralization activity of the complete serum of each animal was set to 100 % and compared to the RBD-depleted sera and the RBD-specific sera.
Therapeutic efficacy of spike-containing VLPs
For further validation, the scientists intranasally and intratracheally challenged the animals with SARS-CoV-2 five weeks after the last immunization with S-containing VLPs. As experimental controls, unimmunized animals were also infected with SARS-CoV-2.
The estimation of genomic and subgenomic viral RNA revealed that, unlike unimmunized animals that showed high viral loads in the upper and lower respiratory tracts, all immunized animals were completely protected from infection with no detectable viral load in the respiratory tract.
Consistent with these findings, no further increase in binding and neutralizing antibody responses was observed in immunized animals following the viral challenge. In these animals, a gradual decline in antibody response was observed from the day of the SARS-CoV-2 challenge to 3 weeks post-challenge.
In contrast, control animals showed a peak neutralizing titer at week 2 post-viral challenge. All immunized animals showed an S-specific CD4+ T-cell response before viral exposure that remained unchanged at day 14 post-exposure. However, no detectable S-specific CD8+ T-cell response was observed in these animals.
Regarding clinical presentations, none of the immunized animals showed abnormal lung pathology. Additionally, these animals maintained stable levels of monocytes after SARS-CoV-2 infection. Comparably, all control animals exhibited mild pulmonary lesions and elevated monocyte levels post-challenge.
Study significance
The current study describes the development of S-containing VLPs that show significant efficacy in inducing sterilizing immunity against SARS-CoV-2. Importantly, these findings demonstrate induction of non-RBD antibodies after the 3rd immunization, which might be beneficial to increase the overall neutralizing efficacy of a vaccine against mutated viral variants. As mentioned by the scientists, non-RBD antibodies are particularly needed to compensate for the loss of RBD-specific neutralization over time.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Sulbaran G., Maisonnasse, P., Amen, X., et al. (2021). Immunization with synthetic SARS-CoV-2 S glycoprotein virus-like particles protects Macaques from infection. bioRxiv. doi:10.1101/2021.07.26.453755. https://www.biorxiv.org/content/10.1101/2021.07.26.453755v1
Posted in: Medical Research News | Disease/Infection News | Pharmaceutical News
Tags: Antibodies, Antibody, Assay, CD4, Cell, Chromatography, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Evolution, Formaldehyde, Genomic, Glycoprotein, immunity, Immunization, Liposomes, Mammalian Cells, Monoclonal Antibody, Monocyte, Pathogen, Pathology, Protein, Pseudovirus, Receptor, Respiratory, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, T-Cell, Vaccine, Virus

Written by
Dr. Sanchari Sinha Dutta
Dr. Sanchari Sinha Dutta is a science communicator who believes in spreading the power of science in every corner of the world. She has a Bachelor of Science (B.Sc.) degree and a Master's of Science (M.Sc.) in biology and human physiology. Following her Master's degree, Sanchari went on to study a Ph.D. in human physiology. She has authored more than 10 original research articles, all of which have been published in world renowned international journals.
Source: Read Full Article






