Sepsis is a potentially life-threatening condition arising from tissue and organ damage due to a body’s overactive response to an infection. Sepsis is commonly characterized by abnormally low levels of platelet (a type of blood cell that can form clots and prevent bleeding), considered to be associated with its high mortality rate.
Recently, Nagoya University researchers and colleagues have shown that a high degree of platelet reduction, rather than an abnormally low platelet count, raises mortality risks in sepsis. The findings, recently published in the journal Scientific Reports, could lead to the development of precise and preventive treatments for sepsis-associated coagulopathy.
It is known that during sepsis, a serious blood disorder called disseminated intravascular coagulation (DIC) forms tiny blood clots throughout the bloodstream, resulting in platelet depletion. From this perspective, absolute platelet count has been used as the international criterion for the diagnosis of sepsis-associated DIC and has led researchers to conduct clinical trials based on this criterion. However, very few of these trials have led to the development of effective treatments for sepsis-associated DIC, and currently, there is no breakthrough therapy.
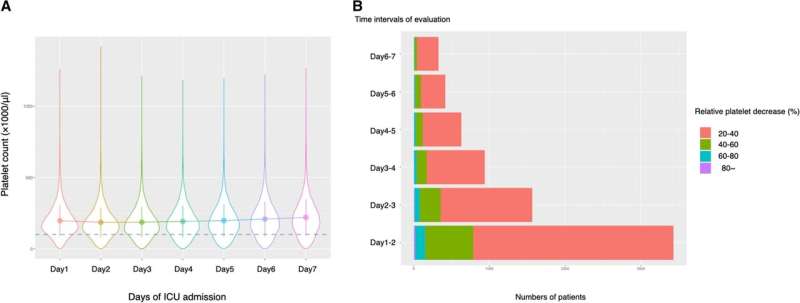
Meanwhile, there has been a theory that the degree of platelet depletion (fast decrease), rather than the absolute platelet count, largely affects mortality risk in sepsis-associated DIC. However, since the evidence for this theory is weak, the degree of platelet depletion has not been considered an international criterion for the disease prognosis.
In this context, Nagoya University researchers and colleagues have conducted a study to examine the significance of the degree of platelet reduction on sepsis mortality rate, using the data of 200,859 sepsis patients staying in intensive care units of 208 hospitals in the United States. “To our knowledge, it was the largest study to evaluate the prognostic impact of both the degree of platelet depletion and absolute platelet counts in patients with sepsis,” says Dr. Daisuke Kasugai of the Nagoya University Hospital, the corresponding author of the study.
The results showed that the degree of platelet reductions correlates with the mortality risk associated with sepsis, regardless of absolute platelet count, indicating that the mortality risk is higher with a fast decrease in platelet count. Dr. Kasugai says, “Surprisingly, we also found that if the platelet count decreases by 11% or more, the risks of bleeding, as well as thrombosis development (a serious condition caused by the formation of blood clots in blood vessels or the heart), increases.”
The researchers have concluded that compared to the absolute platelet count, the degree of platelet reduction could be a more plausible criterion for assessing the mortality risk of the sepsis-associated DIC. They hope that this study will lead to the development of effective treatments for sepsis-associated DIC.
Source: Read Full Article






