The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in December 2019 to cause more than 200 million documented infections and five million deaths. Among the earliest and most characteristic symptoms is olfactory dysfunction due to involvement of the olfactory epithelium (OE). A new preprint shows the persistence of such symptoms after clinical resolution of the infection, hinting at the need for further management.
 Study: Prolonged and extended impacts of SARS-CoV-2 on the olfactory neurocircuit. Image Credit: Design_Cells/ Shutterstock
Study: Prolonged and extended impacts of SARS-CoV-2 on the olfactory neurocircuit. Image Credit: Design_Cells/ Shutterstock
Background
Much research has gone into the mechanism underlying olfactory dysfunction in the coronavirus disease 2019 (COVID-19). Some animal studies suggest extensive patchy shedding of the OE with apoptosis or cellular death, including the olfactory sensory neurons (OSNs), followed by a slow restoration as cells regenerate from the basal cells of the OE.
In humans, however, patients who have recovered from COVID-19 seem to suffer from symptoms affecting the central nervous system (CNS), such as cognitive impairment and depression, along with long-term effects on smell. The current study, which appeared on the bioRxiv* preprint server, looked at the impact of the virus on the CNS in the Syrian golden hamster, a useful animal model for COVID-19.
The OE in the nose is distributed over various locations, with the median-lateral recess and the zone 1-4 areas on the dorsomedial-ventrolateral axis. The areas are restricted by their location as well as sensitivity to noxious agents.
Thus, the toxin methimazole is more noxious to the dorsomedial side, while the lateral side is vulnerable to lipopolysaccharide. The study, therefore, examined the effects of the virus in four regions of the OE: dorsomedial (DM), dorsolateral (DL), ventromedial (VM), and ventrolateral (VL) region.
Following inoculation with the virus into the nose, the six-week-old hamsters were sampled over time for infection in the OE.
What did the study show?
The results showed that several regions within the OE were infected at two days post-inoculation (dpi), clearing by eight dpi. The infected cells extended throughout the DM region thickness. While mature OSNs showed no evidence of infection, the surrounding supporting cells expressing the host cell receptor for the virus, the angiotensin-converting enzyme 2 (ACE2), were positive for the viral antigens.
The VM and VL regions showed a marked drop in supporting cell numbers, while they were unmeasurable in the DM because the OE had been completely lost at five dpi. A near-complete resolution was observed in all regions by 21 dpi.
Sagittal sections of the brain did not show the presence of the viral antigens, not even the olfactory bulb or hippocampus, suggesting that the virus did not enter the parenchyma or did so at undetectable levels. Earlier studies have shown that both the antigens and viral ribonucleic acid can be detected in brain tissue.
The current study showed a short-lived reduction in OE thickness at five dpi, with full recovery by 21 dpi, as with the supporting cells. OSN density remained lower at up to 42 dpi, which could mean delayed or incomplete maturation of these neurons following infection.
The study suggests that the DM region is among the most easily damaged regions after SARS-CoV-2 infection of the OE, probably because of the expression of the ACE2 receptor mostly in these cells. This zone is in zone 1, and the OSNs express the enzyme NAD(P)H quinone oxido-reductase 1 (NQO1).
This useful molecule not only serves as an antioxidant, preventing endocellular oxidation. It is implicated in the generation of reactive oxygen species (ROS) known to enhance nerve cell damage after injury. While cells expressing the maturation marker OMP were fewer after infection, they were restored whether or not they carried NQO1 or not.
Interestingly, more severe damage was found in NQO1-positive regions. After labeling these cells with the ionized calcium binding adaptor 1 (Iba1), macrophage analysis suggested chronic activation in the NQO1-positive regions relative to NQO1-negative regions.
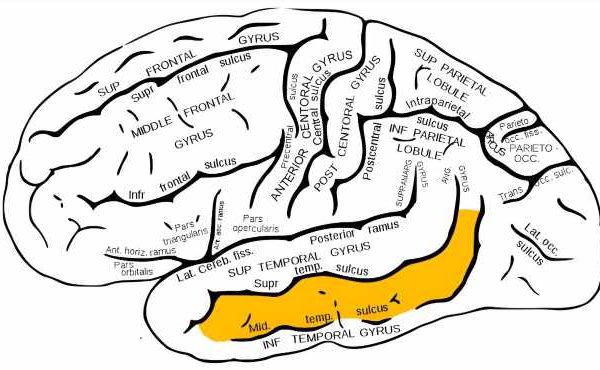
This rapid return to normalcy of the OSNs in the latter region could indicate that the presence of NQO1 is a susceptibility factor for the virus. The same variation in susceptibility was observed within the OB, which serves as the next olfactory relay center, transferring the impulse to the next set of nerve cells.
Here, the synaptic OSN-neuronal connections are found in the form of glomeruli. Within NQO1-positive regions, the OSN axon terminals within the glomeruli were less dense than in the NQO1-negative regions, meaning that the virus could potentially affect how odor signals are processed within the OB, especially the NQO1-positive regions.
The researchers also found that the Iba1 signal was strongest in all OB layers at 17 dpi, whereas it was highest at five dpi in the OE. This could mean that microglial activation in the OB was at a lower rate than in the OE macrophages.
At five dpi, activation signals were strongest in the olfactory nerve layer (ONL), where the OSN axons are densely packed. This could indicate microglial responses to OSN axonal injury occurred rapidly and directly in the ONL.
Conversely, this damage is an indirect signal on post-synaptic neuronal circuits in the glomerular layer (GL, where the OSN axons make synaptic connections with relay neurons) and the external plexiform layer (EPL), where projection neurons synapse with the interneurons.
In agreement with these findings, the NQO1-positive regions showed greater damage at five dpi, but only at 17 dpi within the GL than NQO1-negative regions. At 17 dpi, a larger area was occupied by glial fibrillary acidic protein (GFAP)-expressing astrocytes in the GL, independent of NQO1 expression.
In other words, microglial activation in the GL is linked to astrocyte activity more strongly than in other layers.
GFAP signals were short-lived in the pia mater but appeared over a longer period in the first layer of the piriform cortex (PC), a higher brain area. Iba1-expressing activated microglia in the pia mater were more abundant at both five and 17 dpi, but the area covered by these cells remained the same in layer one.
There was no association between the presence of the virus in the nose and the peak activity in the brain, which could mean that activation of microglia in the PC is indirect via local or systemic inflammation. This is borne out by the elevation of inflammatory cytokines in the bloodstream following SARS-CoV-2 infection.
Infection is likely to be present in the lamina propria of the OE since it expresses ACE2 and shows evidence of macrophage activation in infected animals. The authors postulate that the immune response to the virus in this layer is responsible for the systemic inflammatory response. This may, in turn, cause microglial activation in the CNS.
In the hippocampus, GFAP-positive astrocytic endfeet were found in abundance, clustered around the blood vessels of the apical dendritic region, at five, eight, 17, and 42 dpi. While Iba1 expression peaked at eight dpi, in the basal region, it reverted to normal at 42 dpi, unlike in the apical region. The virus appears to have led to the activation of the microglia and astrocytes, even in the hippocampus, but with different impacts per layer.
Glial cells can modulate synaptic transmission or cause synaptic loss, induce synaptic plasticity and change synaptic density, and these actions are sometimes linked to demential changes. To examine this possibility, the researchers found basal dendritic spines to be very stable in the hippocampus, while the apical spines showed a marked fall in density. This may be associated with persistent microglial activation, especially marked at 42 dpi.
What are the implications?
Overall, the study shows that vaccination with a single dose of SARS-CoV-2 caused long-lasting effects on the OE and brain regions concerned with normal cognitive function. Glial cells were activated and synaptic transmission altered in the absence of any direct effect of the viral antigens, as shown by their absence in the CNS.
The effect of these changes on animal behavior, and the time required to recover from them, may be elucidated in future studies, which will help uncover the mechanisms of olfactory loss and perhaps cognitive impairment following recovery from COVID-19.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information
- Kishimoto-Urata, M. et al. (2021). Prolonged and Extended Impacts Of SARS-Cov-2 On the Olfactory Neurocircuit. bioRxiv preprint. doi: https://doi.org/10.1101/2021.11.04.467274. https://www.biorxiv.org/content/10.1101/2021.11.04.467274v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Animal Model, Antioxidant, Apoptosis, Astrocyte, Blood, Blood Vessels, Brain, Calcium, Cell, Central Nervous System, Chronic, Cognitive Function, Coronavirus, Coronavirus Disease COVID-19, Cortex, Cytokines, Depression, Enzyme, Hippocampus, Immune Response, Inflammation, Macrophage, Microglia, Molecule, Nerve, Nervous System, Neurons, Oxygen, Protein, Receptor, Research, Respiratory, Ribonucleic Acid, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Synapse, Syndrome, Toxin, Virus

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article