Biologics, a class of therapeutics derived from living organisms, offer enormous advantages to patients battling challenging diseases and disorders. Treatments based on biologics can boost the immune system to stem attacks from infections or target specific pathways to block the formation of tumors.
“These drugs, which have been around for just the last 20 years, do magic,” says Amir Erfani, a postdoc in the MIT Department of Chemical Engineering (ChemE). “They can save millions of people around the world.”
But the unrivaled effectiveness of biologics comes at a cost. They can be difficult to administer, often demanding time-consuming intravenous (IV) infusions at clinics. Whether for patients struggling with life-threatening or lifelong conditions, the prospect of spending hours away from home, every few weeks, can prove extremely daunting.
Now, new work from an MIT team in collaboration with the Merck pharmaceutical company suggests a practical solution for surmounting the difficulty of administering biologics. In a recent paper published in Advanced Healthcare Materials, these researchers describe a hydrogel platform for delivering monoclonal antibodies (MABs)—one type of biologic—through subcutaneous injection.
Erfani is lead author of the paper. Co-authors include Jeremy M. Schieferstein, a postdoc in ChemE at the time of the study, now senior scientist at Elektrofi; Apoorv Shanker, a postdoc in ChemE; Paula Hammond, Institute Professor and head of ChemE; and Patrick S. Doyle, the Robert T. Haslam (1911) Professor of Chemical Engineering, as well as Merck researchers.
“This is an important milestone,” says Doyle. “We are on the route to transforming the next generation of treatment with monoclonal antibodies and other kinds of therapeutics.”
Higher-test antibodies
Unlike most conventional drugs that are formulated chemically and comprised of small molecules, biologics are sprawling and unruly chains of proteins, sugars, and DNA segments, genetically engineered from living sources. These giant organic molecules don’t lend themselves to the kind of neat, dense packaging typically found in synthesized pills or injectable suspensions.
Take the MAB on which Erfani and Doyle focused, called pembrolizumab, or pembro for short. This unique antibody binds to a receptor associated with mediating immune responses to tumor cells, and is used in a range of sometimes intractable cancers. Pembro is normally administered in a dilute solution by IV over several hours to achieve the kind of concentrations required to be effective. (Merck has patented this formulation of the drug as Keytruda.)
“When you try to concentrate existing formulations, the molecules’ viscosity grows astronomically,” says Doyle. “At a critical point, they start almost feeling for each other, and interact to become a kind of paste.” Forced together, pembro molecules become unstable and change their structure, undermining their therapeutic properties.
So Doyle’s team of researchers in the Soft Matter Engineering Group set about creating a version of pembro that could be injected at high enough concentrations to be effective, but in small enough volumes to be administered comfortably and swiftly just under the skin (the second preference of most patients and clinicians, after swallowing a pill). With expertise in matters of flow, microfluidics, and pharmaceutical formulations, the lab was well-equipped for the challenge.
Go with the flow
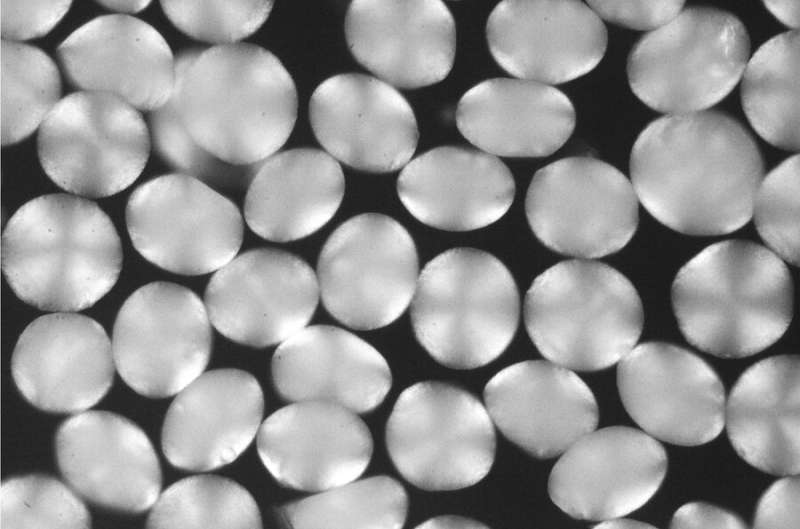
“This MAB is super sticky and delicate, and we needed to find some way to get its molecules moving freely inside a syringe,” says Erfani. “The insight we had was to use hydrogel particles, made from sugar-based, water-loving biopolymers that provide a nice environment where a protein is going to be very happy,” says Doyle. “We’d used these for other applications, and I knew if we could make them small enough, they could get through a needle without clogging it.”
The researchers knew from toxicity literature that their hydrogel capsules would be biocompatible, and would behave in a syringe. “The hydrogel particles are squeezy, and can roll over each other, and actually flow,” says Erfani. It looked like clear sailing to incorporate pembro molecules at the right density for a one- to two-millimeter subcutaneous injection. But, like so much in engineering, the devil turned out to be in the details.
“It was tricky keeping the antibody intact through the fabrication process, and then ensuring it could be biologically effective as it dispersed properly under the skin,” says Doyle. Any departure from the precise formulation of the pembro integrated into the soft hydrogel capsules might render the MAB ineffective, or worse.
In a series of experiments lasting nearly five years, Doyle’s lab experimented in achieving just the right balance of features. Their studies relied on a homemade device that jets out biopolymer solution and crystals of pembro together first into the air, and then into a bath where they fuse into beads.
“We tested many variables in our design space,” says Erfani, including different concentrations of pembro, and the composition and pH of the polymer solutions. “The goal wasn’t just developing a drug in our lab, but developing a process that could be easily adapted to pharmaceutical manufacturing.”
With his prior industry background developing types of MAB in stable, crystalline structure, Erfani helped push the team over the finish line. “He not only brought all this physical chemistry to the process, but he figured out the experimental design and how to execute on it,” says Doyle.
A broad platform
The researchers are now putting their pembro formulation through its paces through in vivo trials, with the aim of U.S. Food and Drug Administration approval in the next few years. But Doyle and his group have broader goals for the hydrogel platform they invented. “We believe this platform is agnostic to the MAB, which means we can get a lot of different molecules formulated to the right concentration and flowability,” he says. “That’s a big deal.”
Among the possibilities Doyle envisions are a slow, sustained release of the MAB-containing hydrogel particles—think weeks—after injection. The platform could accommodate other kinds of molecules, such as cytokines, to amplify immune response, or target specific cancer pathways. Hydrogels could also incorporate two kinds of drugs that enhance each other’s properties.
Erfani points to the potential social impacts of the platform. “Our technology holds the possibility of improving the accessibility of treatments by reducing a patient’s dependency on hospitals,” he says. Replacing IV sessions with fewer, single-shot injections would free up time in clinics for more patients, encourage greater compliance, and even lower the price of the drug, he notes. People might someday administer their own injections at home.
Erfani is especially intrigued by the notion of moving many more drugs to this platform, including some that died early in development. “There are drugs companies that gave up because they couldn’t be formulated in high enough concentrations,” he says. “Wouldn’t it be super exciting to repurpose a lifesaving drug and bring it back to market?”
More information:
Amir Erfani et al, Crystalline Antibody‐Laden Alginate Particles: A Platform for Enabling High Concentration Subcutaneous Delivery of Antibodies, Advanced Healthcare Materials (2023). DOI: 10.1002/adhm.202202370
Journal information:
Advanced Healthcare Materials
Source: Read Full Article






