Reports of new variants of the SARS-CoV-2 coronavirus have become more frequent in the last few weeks. Richard Neher researches the evolution of viruses and bacteria at the Biozentrum of the University of Basel. From 2011 to 2017, he was a research group leader at the Max Planck Institute for Developmental Biology in Tübingen.
Professor Neher, coronaviruses were previously considered a comparatively stable group. How is it that variants are now appearing more frequently?
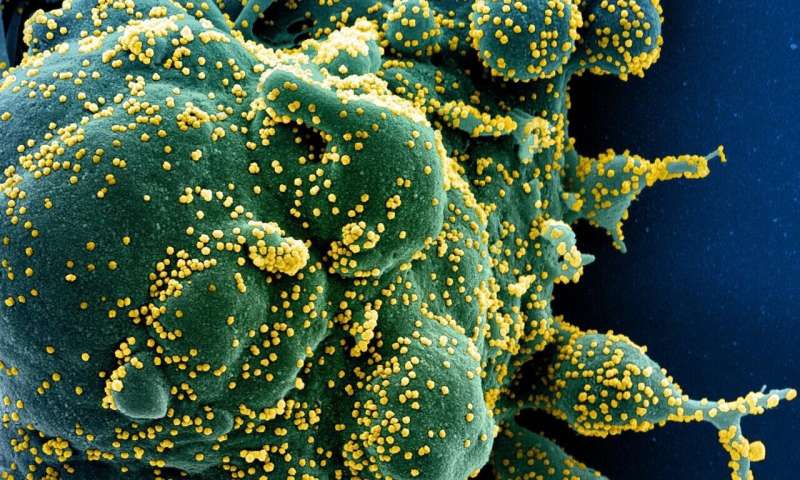
SARS-CoV-2 mutates less quickly than flu viruses or HIV, but the differences are not that considerable. The resulting genetic lines enable us to reconstruct the propagation paths of the virus. But until recently, there was little evidence that these mutations greatly alter the properties of the virus.
It has now been shown that some variants spread faster than others. Preliminary results from cell cultures also indicate that antibodies are less able to recognize certain virus strains. However, we do not yet know whether this will actually have an effect on immunity.
In some variants five, ten, or even more mutations appear at once. I would not have expected that.
How do you explain the rapid evolution?
It may indicate increasing and persistent selection pressure. For example, an increasing degree of immunity in the population favors virus variants that can partially escape the body’s defenses.
Under what conditions can such selection pressure arise?
It can occur at the level of an individual or a population. For example, in individuals with weakened immune systems, who cannot effectively fight the virus effectively, the pathogen can “try out” new things for a longer period of time. In the end, the variants that most effectively escape the body’s defenses remain.
Regions where the first wave of the pandemic was particularly strong—such as parts of South America and South Africa—also exert strong selection pressure because many people there developed immunity following SARS-CoV-2 infection. New virus variants may have an advantage here.
In South Africa and Brazil, researchers have been closely following the development of the virus. These remarkable variants were therefore discovered and studied early on. In other places, there may be similar variants that we don’t know about yet.
Can populations develop herd immunity against SARS-CoV-2 under these circumstances?
Probably not globally—but locally for a certain time if the vaccination rate is high. The viruses change too quickly for herd immunity to develop permanently in the population.
Could COVID-19 cause death rates similar to those of SARS-CoV—which appeared in southern China at the end of 2002—through new variants? After all, the SARS virus from back then is related to today’s SARS-CoV-2.
We have no reason to expect such a thing. SARS-CoV and SARS-CoV-2 have been diverging for a long time and are thus clearly different from each other at the genetic level. These differences go far beyond the extent of the mutations we have observed so far. Therefore, in my opinion, it is highly unlikely that COVID-19 will cause death rates similar to SARS-CoV did in 2002/2003.
Will we need to be vaccinated against COVID-19 every year in future just like we do against influenza?
Source: Read Full Article






