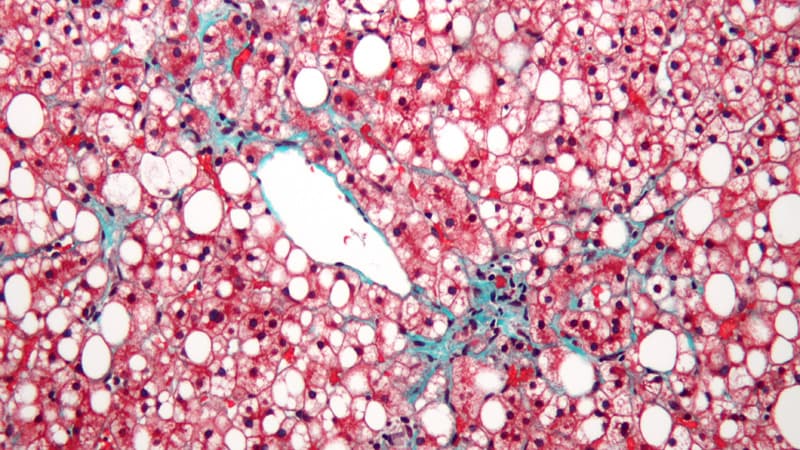
LONDON — Resmetirom (Madrigal Pharmaceuticals) is a safe option for patients with nonalcoholic steatohepatitis (NASH), according to a pair of studies sharing results from the phase 3 MAESTRO NAFLD-1 trial. Not only was the investigational, oral, liver-directed, selective thyroid hormone-receptor beta-agonist well tolerated, its use led to reductions in liver fat, fibrosis, atherogenic lipids, and liver volume by approximately 20%.
Results from the 52-week double-blind, placebo-controlled study of resmetirom were presented by Stephen Harrison, MD, medical director for Pinnacle Clinical Research in San Antonio, Texas, and principal investigator of the MAESTRO studies, at the International Liver Congress (ILC) 2022.
“The positive results from MAESTRO-NAFLD-1 support our conviction that resmetirom has the potential to be the first medication approved for the treatment of NASH with significant liver fibrosis,” asserted Harrison. “Both safety/tolerability and efficacy are required for a drug to obtain approval by the US Food and Drug Administration and European Medicines Agency,” noting that with these recently announced resmetirom results, “half of the equation is now met.”
Results From the Primary Analysis: Safety First
In the first of two oral presentations, Harrison shared results from the MAESTRO-NAFLD-1 trial’s primary analysis. It included 1143 patients (mean age, 55.9 years; 49% with type 2 diabetes) in the United States, randomly assigned equally to once-daily resmetirom doses of 80 mg, 100 mg, and placebo. Additionally, 171 patients went on to receive open-label 100 mg resmetirom (cirrhotic and noncirrhotic arms) after completing the first part of MAESTRO-NAFLD-1.
Patients had at least three metabolic risk factors (metabolic syndrome), a FibroScan kPa of 5.5-8.5, and a controlled attenuation parameter (CAP) ≥ 280. MRI proton density fat fraction (MRI-PDFF) showed that the percentage liver fat was approximately 17%-18% across all groups.
The primary objective at 52 weeks was safety and tolerability vs placebo, as measured by incidence of adverse events. Treatment-emergent adverse events were seen in 88.4%, 86.1%, and 81.8% of patients receiving resmetirom 80 mg, 100 mg, and placebo, respectively. Serious treatment-emergent adverse events were seen in 6.1%, 7.4%, and 6.3%, respectively. Study discontinuations as a result of drug-related adverse events were 1.5%, 1.9%, and 0.9%, respectively.
The most frequent adverse events were gastrointestinal related (diarrhea and nausea), though there was no increase in the incidence of GI-related adverse events after the first 12 weeks of resmetirom treatment.
Aleksander Krag, MD, PhD, professor and senior consultant of hepatology and director of Odense Liver Research Centre at the University of Southern Denmark and Odense University Hospital, Denmark, commented on the findings to Medscape Medical News.
“We see a lot of drugs failing because of lack of safety,” said Krag, also vice secretary of the European Association for the Study of the Liver. “It’s interesting because this is a huge trial just on safety primarily. Based on this, we can say that resmetirom is safe because this trial was in over 1000 people and involves a long period of treatment looking at the safety profile.”
Secondary Results Attest to Efficacy
MAESTRO-NAFLD-1 does not include a liver biopsy and represents a ‘real-life’ NASH study. Instead, NASH or presumed NASH is determined using historical liver biopsy or noninvasive techniques, including FibroScan and MRI Proton Density Fat Fraction (MRI-PDFF).
The study aimed to identify secondary noninvasive efficacy markers that correlate with individual patient response to resmetirom, including LDL-C (change at week 24), apolipoprotein B (APOB) at week 24, hepatic fat fraction (MRI-PDFF) at week 16, triglycerides (TG) at week 24, and FibroScan CAP Vibration Controlled Transient Elastography (VCTE) at week 52.
The main secondary endpoints were achieved for both 80 mg and 100 mg groups (P < 0.0001 for LDL-C, APOB, MRI-PDFF, TG, and FibroScan CAP). LDL-C, APOB, and TG dropped by -14.4%, -16.6%, and -21.5%, respectively, at week 24 in the 100 mg group.
MRI-PDFF at week 16 and at week 52 and FibroScan CAP at week 52 were -48, -48, and -42, respectively, also in the 100 mg group.
Lipid reductions were numerically greater in the 100 mg open-label arm compared with the 100 mg double-blind arm, remarked Harrison.
The study was conducted from December 2019 to November 2021 during the height of the COVID-19 pandemic.
“Patients in the open-label 100 mg arm were less impacted by COVID-related dose interruptions than double-blind patients,” he noted. “MRI-PDFF reductions were robust, even though some double-blind patients had COVID-related treatment interruptions.”
“Equally important, when we think about noninvasive tests, is magnetic resonance elastography (MRE), which measures fibrosis change,” added Harrison. “Here we saw a significant difference between the drug-treated groups and placebo. In fact, when we look at the responder analysis, they improved their MRE by at least 19%. We doubled that rate compared with placebo.”
“These results are not registration efficacy results, but they certainly support movement in a positive direction in terms of liver biopsy,” he said.
In terms of fatty liver, “we have reduced liver fat significantly, so that at 16 weeks it was around 43%, increasing to around 49%-50% by week 52,” Harrison said, adding that liver chemistry tests “all moved in a positive direction.”
Krag remarked of the noninvasive secondary measures: “They found a clear signal between dosing and MRI-based effects. I think for the company, it was confirmation of safety, and for us, as a liver-treating community, patient safety must come first.”
Results From the Open-Label Analysis
In a second presentation, Harrison shared results from the open-label arm of the MAESTRO NAFLD-1 trial.
In this analysis, 105 patients (mean age, 62.7 years) who had F4 disease or F2/3 disease on biopsy with clinical progression were enrolled. Patients had well-compensated Child-Pugh class A scores (5-6 points). Baseline FibroScan VCTE was kPa 24.6, MRE was 5.7, mean ALT was 40, and mean AST was 39. These values were consistent with F4 fibrosis.
The study also had a 52-week duration and included multiple exploratory endpoints, among them serum lipids, liver chemistry tests, some noninvasive markets of liver fat and fibrosis, but also liver volume and spleen volume, as well as safety.
“The marked reductions in noninvasive measures of fibrosis, liver fat, and liver volume observed at 52 weeks in the open-label cirrhosis portion of the trial are particularly encouraging because this is a difficult-to-treat population at elevated risk of progressing to negative outcomes,” said Harrison.
Patients with lower MRI-PDFF (≤ 5%) at baseline had more progressed cirrhosis and greater spleen volumes. Similar to patients with noncirrhotic NASH, liver volume was greatly elevated compared to normal at baseline.
“This was a definite cirrhotic population by any noninvasive test,” said Harrison.
Resmetirom reduced MRI-PDFF and LDL-C and other atherogenic lipids in the patients with NASH cirrhosis, and reduced FibroScan CAP, VCTE, and MRE in a significant fraction of patients. The largest reduction in FibroScan VCTE, with a mean reduction of 9 kPa, occurred in the more advanced group (baseline PDFF ≤ 5%). Similar improvements were observed in MRE.
By week 52, 73% of patients, independent of baseline cirrhosis severity, had at least 15% reduction in liver volume. Spleen volume was also reduced and was strongly correlated with liver volume change and exposure to resmetirom.
“This drug was found to be well-tolerated and safe in this population of well-compensated Child-Pugh [class] A patients,” commented Harrison.
Mild GI adverse events were seen at the beginning of therapy. There were no differences seen in safety parameters between patients with cirrhosis compared with noncirrhotic NASH patients, and there were no thyroid axis changes or hyper- or hypothyroid symptoms observed.
Harrison concluded that the drug was safe and well tolerated, and there was significant improvement in liver fat content and atherogenic lipids, as well as positive improvements in AST, ALT, and gamma-glutamyl transferase.
More Resmetirom Studies to Come
MAESTRO-NAFLD-1 is one of two phase 3 studies of resmetirom, the other being the ongoing phase 3 MAESTRO-NASH trial that is looking at the treatment of NASH with fibrosis in up to 2000 patients, and uses double-blind 80 mg and 100 mg resmetirom, as well as placebo over 52 weeks.
The already-published phase 2b trial showed that 36 weeks of resmetirom improved liver fat content significantly and also correlated with significant resolution of NASH.
Later this year, final results of the registration MAESTRO-NASH trial on efficacy will be reported. Together, it’s intended that the MAESTRO phase 3 trials provide a comprehensive dataset to support accelerated approval of resmetirom for treatment of NASH with significant liver fibrosis, Harrison pointed out.
Harrison discloses the following:
Scientific advisor or consultant for Akero, Altimmune, AstraZeneca, Axcella, Echosens, Galectin, Gilead, GSK, Hepion, HistoIndex, Intercept, Madrigal, Medpace, Metacrine, NGM Bio, Northsea, Novartis, Novo Nordisk, PathAI, Poxel, Sagimet, Sonic Incytes, Terns, and Viking.
Stock options: Akero, Cirius, Galectin, Genfit, Hepion, HistoIndex, PathAI, Metacrine, NGM Bio, and Northsea.
Grant/research support: Akero, Altimmune, Axcella, BMS, Cirius, CiVi Biopharma, Conatus, Cymabay, Enyo, Galectin, Genentech, Genfit, Gilead, Hepagene, Hepion, Hightide, Intercept, Ionis, Madrigal, Metacrine, NGM Bio, Novartis, Novo Nordisk, Northsea, Pfizer, Sagimet, Viking, 89 Bio.
Krag reports no relevant financial relationships.
International Liver Congress (ILC) 2022. Abstracts LB005 and OS121. Presented June 25, 2022.
For more news, follow Medscape on Facebook, Twitter, Instagram, YouTube, and LinkedIn
Source: Read Full Article