Antibiotic resistance surveillance in the Philippines has moved into the genomic era, enabling better tracking of dangerous bacteria. Researchers at the Centre for Genomic Pathogen Surveillance (CGPS housed at the Wellcome Sanger Institute and The Big Data Institute (BDI), University of Oxford), and the Philippine Research Institute for Tropical Medicine (RITM), set up local DNA sequencing and analysis of drug resistant bacteria in the Philippines. This genomic capacity has enhanced ongoing national infection control including tracking the spread of resistance to last-line antibiotics and identifying drug resistant infections in a hospital baby unit, helping control the outbreak.
Reported in Nature Communications this week, this study shows the power of local genomic sequencing within national surveillance networks in low- and middle-income countries, and could be extended to other locations to tackle the global challenge of antimicrobial resistance.
Antimicrobial resistance (AMR) is a global health problem, with resistance to common antibiotics found in all regions of the world. This means it can be extremely difficult to treat some bacterial diseases such as MRSA, tuberculosis and gonorrhoea, and raises risks of any surgery.
Surveillance of AMR is critical to understand and try to halt its spread, and DNA sequencing can pinpoint resistance mechanisms and uncover transmission patterns. However, genomic surveillance is less common in low- and middle-income countries (LMICs), which are predicted to be the most affected by AMR.
The Philippines has a very well established Antimicrobial Resistance Surveillance Program within the Philippine Department of Health, which uses laboratory-based methods to track antimicrobial resistance. In 2018 the researchers helped set up a DNA sequencing facility within this to build local capacity for genomic surveillance in the Philippines. This has included establishing local capacity in genomics and data interpretation through shared training.
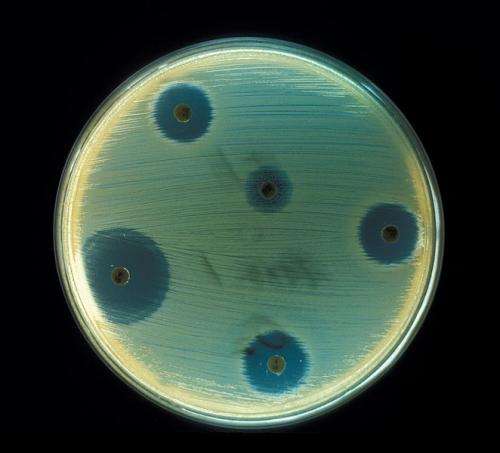
Samples were sequenced from more than 20 sites across the Philippines, focusing on bacteria that are resistant to the last-line antibiotics, and listed by the World Health Organisation as top priority pathogens for the development of new antibiotics. The teams collectively analysed the data, creating phylogenetic trees that showed how the bacterial strains are related to each other, and uncovered several high-risk clones.
Combining the genetic findings with epidemiological data allowed the researchers to pinpoint strains in particular locations. In one hospital they identified a cluster of the same strain of carbapenem-resistant Klebsiella pneumoniae in a neonatal intensive care unit, and revealed that this was being spread within the hospital. This evidence enabled the hospital to bolster their infection control team, to control potential future outbreaks.
Dr. Celia Carlos, joint lead of the project from the Research Institute for Tropical Medicine, Philippines, said: “Here in the Philippines we have more than 30 years of experience developing laboratory methods to track AMR, with our Antimicrobial Resistance Surveillance Program. Now, working with our partners in the UK, we have established local capacity and expertise for whole genome sequencing in the Philippines, adding genomic surveillance to these other methods. This is helping us to identify emerging resistant strains much faster, so we can understand what is happening, prevent transmission of AMR and save lives.”
Dr. Silvia Argimón, first author on the paper from the Centre for Genomic Pathogen Surveillance said: “The programme not only helped set up the genomic infrastructure in the Philippines, but also enabled close collaboration between the teams in the UK and the Philippines. This included exchange visits between the researchers and training to transfer ownership of the sequencing, analysis and understanding to the team in the Philippines, and ensured that everyone understood the resourcefulness and challenges of the sentinel sites.”
Genomic surveillance allows the team to describe drug-resistant bacteria in terms of their strains, which genes enable the resistance, and how those genes are transferred between bacteria. Through genomics the Philippines now have a greater lens on AMR at the local, the national and international scale, allowing data analysis at a previously difficult level. The data are shared with Philippine public health agencies and with the WHO to inform both local and global understanding of the spread of carbapenam resistance.
Source: Read Full Article






