MRI criteria used to diagnose axial spondyloarthritis (axSpA) may require gender-specific revision, according to research conducted at Charité Universitätsmedizin Berlin.
Although established MRI markers were detected in both sexes, their prevalence was substantially different in some cases — ankylosis and fat metaplasia were more prevalent in male than female patients, for example, while sclerosis was far more common in females.
“There’s increasing evidence in the literature and awareness in clinical practice that there are some sex differences in the clinical presentation of axSpA,” said radiologist Sevtap Tugce Ulas, MD, at the annual European Congress of Rheumatology.
She presented the first results of a study examining the diagnostic performance of MRI findings for men and women. “Men have a high risk of structural damage, while women are more likely to be affected by peripheral manifestations with a higher risk for pain, stiffness, and fatigue.”
Joint biomechanics are different in men and women, she pointed out, which might explain some of the disparities. She observed that diagnostic delay – a known problem in axSpA — was “significantly longer” in female patients.

Dr Sevtap Tugce Ulas
Ulas and colleagues conducted a post hoc analysis of participants in six prospective axSpA cohorts. From a total of more than 1,100 participants, the researchers identified 684 who had both a clinical diagnosis and complete imaging data available for evaluation. The study population included 379 men and women with and 305 men and women without axSpA.
The mean age overall in all groups was 37 years, with axSpA patients more likely than controls to have elevated C-reactive protein levels; levels were also higher in men with axSpA, compared with in women with axSpA.
Men with axSpA also were more likely than women to be HLA-B27 positive (91% vs. 79%), but there were similar mean Bath Ankylosing Spondylitis Disease Activity Index scores recorded (4.4 vs. 4.6) among the subjects with axSpA.
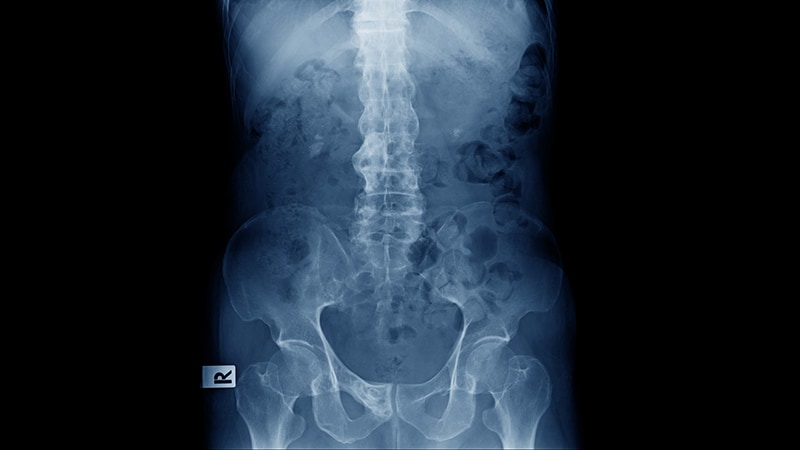
Two experienced radiologists, blinded to the clinical diagnosis, scored the MRI images independently of each other, looking for the presence of ankylosis; erosions; sclerosis; fat metaplasia; and bone marrow edema in the ventral, mid, and dorsal regions of the sacroiliac joints. Any disagreement between the two reviewers was assessed by a third, more experienced radiologist.
Clear Differences in MRI Markers
“If you look in detail, we found no major sex-specific differences for erosion and bone marrow edema,” Ulas reported.
The situation was quite different for other MRI parameters examined. Indeed, more men than women had evidence of ankylosis (24.3% vs. 7.4%) and fat metaplasia (58.8% vs. 42.6%). Conversely, women were more likely than men to have evidence of sclerosis (75.0% vs. 57.6%).
“To make the performance more easily comparable, we calculated a diagnostic odds ratio, which is simply positive likelihood ratio divided by negative likelihood ratio,” Ulas said.
Doing this showed that the presence of ankylosis had “an almost 10 times stronger performance in men,” with a DOR of 40.1 versus 4.7 for women.
“Interestingly, this was not only caused by low prevalence in females, but also by high rates of false positives,” she said.
DOR for the other parameters in men and women were 18.6 and 6.3 for fat metaplasia, 2.5 and 3.0 for sclerosis, 17.6 and 11.1 for joint erosion, and 2.5 and 3.7 for bone edema.
Overall, diagnostic accuracy was improved only when middle and dorsal lesions were considered.
“Remarkably Different” Results
“By definition, these patients have the same disease,” said Hendrik Schulze-Koops, MD, of Ludwig Maximilian University of Munich (Germany).
Yet these are “remarkably different” findings, Schulze-Koops said during a closing highlights session of the congress.

Dr Hendrik Schulze-Koops
Current imaging practices don’t differentiate between the sexes but perhaps they might need to, he said, because these data suggest “female patients have a different MRI pattern from what we learn from the textbooks.
“[The investigators] say diagnostic performance of established imaging markers on MRI is significantly lower in female axSpA patients, and we should consider this when we are in the situation where we question the disease.”

Dr Marta Mosca
Marta Mosca, MD, PhD, of the University of Pisa (Italy) and who cochaired the session in which Ulas had presented the findings commented: “I think is very interesting. We always talk about gender differences in treatment and in the assessment.”
However, Mosca asked if there were plans to study other patient cohorts, notably those not just referred by a rheumatologist, as that was “a big limitation.”
Ulas replied: “I think we need follow-up studies to investigate this problem, because we know that there are differences in the clinical presentation and also in the imaging, and this is an important point.”
Of course, there are other limitations, Ulas said, such as the sole use of conventional T1-weighted spin echo sequences. Although often routinely used in clinical practice, this imaging technique can lead to overestimation of structural damage. Moreover, “subtle differences might have been missed” in bone marrow edema because it wasn’t included in the semiquantitative scoring system used.
“Most importantly, the MRI images under investigation were also used in the diagnostic process, which carries the risk of circular reasoning,” Ulas said.
However, there are clearly some differences in imaging appearance between men and women, and “we show a significantly lower performance of many typical MRI findings in women,” Ulas said. “We hope that these findings might spark a critical discussion on the appropriateness of sex-blind classification criteria for axSpA, and hopefully, eventually lead to refined criteria for both sexes.”
Ulas had no conflicts of interest to disclose. Schulze-Koops and Mosca were not involved in the study and had no relevant disclosures.
This article originally appeared on MDedge.com, part of the Medscape Professional Network.
Source: Read Full Article