
A team of researchers in biomedical engineering, mechanical engineering and biomechanics in Ireland, the Netherlands and the U.S. recently developed 3-D bioprinted implants optimized with growth factors to facilitate angiogenesis—blood vessel growth from existing vasculature—and osteogenesis—new bone growth. In this work, Fiona E. Freeman and colleagues functionalized bio-inks with nanoparticles to print implants with distinct growth factor patterns and noted how the rate of in vivo blood vessel growth (angiogenesis) depended on the expression of the vascular endothelial growth factor (VEGF). They noted higher levels of vessel invasion in implants containing a gradient of VEGF compared to those homogeneously loaded with similar amounts of the protein. The printed implants maintained a gradient of VEGF coupled with spatially defined bone morphogenetic protein (BMP) localization and release kinetics to accelerate large bone defect healing alongside minimal heterotopic bone formation i.e. abnormal bone growth in nonosseous tissue. The work has potential to bioprint growth factors for point of care therapy and in biomedical applications of tightly controlled tissue regeneration.
Growth factors for therapeutic applications
Researchers have tested a number of growth factors in clinical trials for varying therapeutic applications including bone regeneration and new blood vessel formation or neovascularization. Despite promising results, some outcomes in phase two-trials have not shown expected benefits to patients and some have even demonstrated marked adverse effects. Growth factors are typically expressed during different phases of fracture healing, including vascular endothelial growth factor (VEGF) and bone morphogenetic protein (BMP). For optimal outcomes scientists have developed combination therapies of the two growth factors (VEGF and BMP) to accelerate the regeneration of large bone defects. During fracture healing, the BMP-2 expression levels typically increase constantly until day 21, while VEGF expression peaks earlier. Therefore, they developed delivery systems that supported the early release of VEGF and the sustained release of BMP-2. In this work, Freeman et al. used multiple-tool biofabrication techniques to deliver VEGF and BMP-2 with distinct release profiles to improve regeneration of critically sized bone defects.
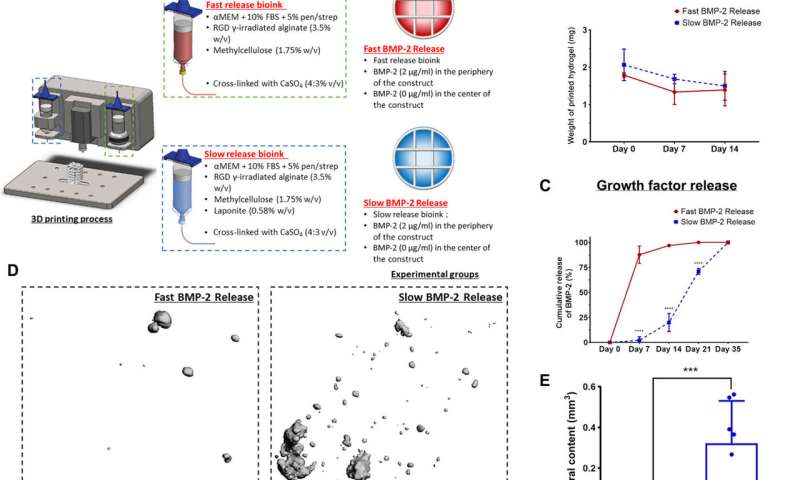
Developing bioinks with distinct growth factor release profiles for in vivo implantation
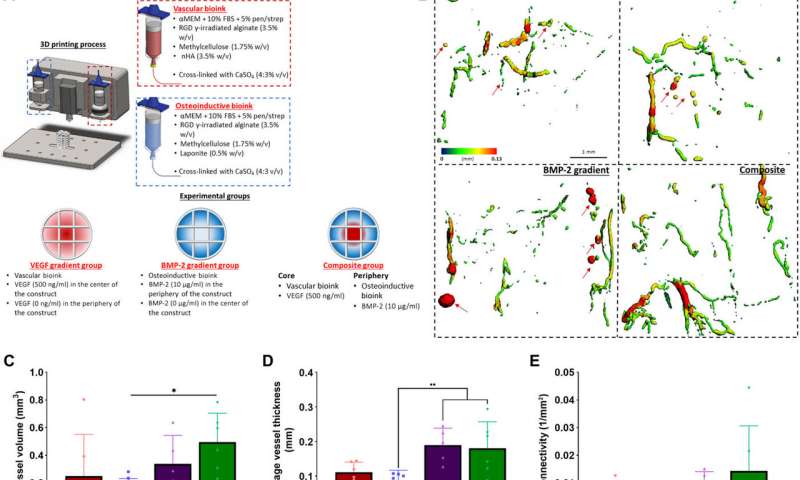
The team controlled the release of morphogens (growth factors) from 3-D printed constructs, which they developed with alginate-based bioinks with different nanoparticles embedded to bind the regulatory factors. They slowed the release of BMP-2 in the constructs to enhance in vivo bone formation in predefined locations of the implant for accelerated bone healing while minimizing ectopic bone formation. Freeman et al. used clay nanoparticles or hydroxyapatite nanoparticles in the bioink made of alginate-methylcellulose to facilitate controlled VEGF release. They showed how the constructs maintained spatial gradients of growth factors for at least 14 days in the lab after bioprinting.
The printed VEGF constructs enhanced angiogenesis in vivo, which the team tested by depositing the constructs in 3-D printed polycaprolactone (PCL) implants to accelerate vascularization in a mouse model. Two weeks after subcutaneous implantation within the animal model, they conducted histological analyses to reveal the presence of vessels in homogenous and gradient VEGF groups. There were no obvious vessels present in the no VEGF group. Between two to four weeks, the gradient VEGF groups had significantly higher vessels in the periphery constraints, Freeman et al. noted the vessel growth in constructs to be mature and complete.
Delivering BMP-2 to localize bone formation in vivo
Since the slow and sustained release of BMP-2 is known to contribute to optimal bone regeneration, the team conducted bone formation studies in a mouse model with growth factor release within a distinct time-frame. To markedly reduce the release of BMP-2 from the bioink, Freeman et al. added laponite (a nanomedicine platform) and monitored its constant release from one to four weeks in the lab. To then understand the effects on bone formation (osteogenesis) in an animal model, the scientists constructed bioinks for fast BMP-2 release (without laponite) and slow BMP-2 release (with laponite) and mixed the bioinks with bone marrow-derived mesenchymal stem cells (BMSCs) and deposited them within 3-D printed scaffolds. They then implanted these scaffolds subcutaneously in the back of mice and followed the process by seeding additional mesenchymal stem cells to test bone growth in an ectopic location. Quantification studies showed the slow release of BMP-2 for significantly more new bone formation per total area of the construct. The work also showed the slow release of BMP-2 to have significantly more new bone forming potential per total area of the construct.
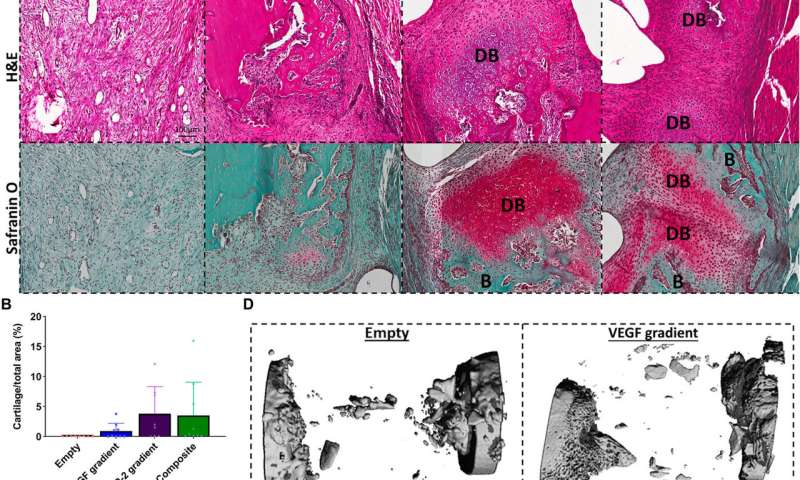
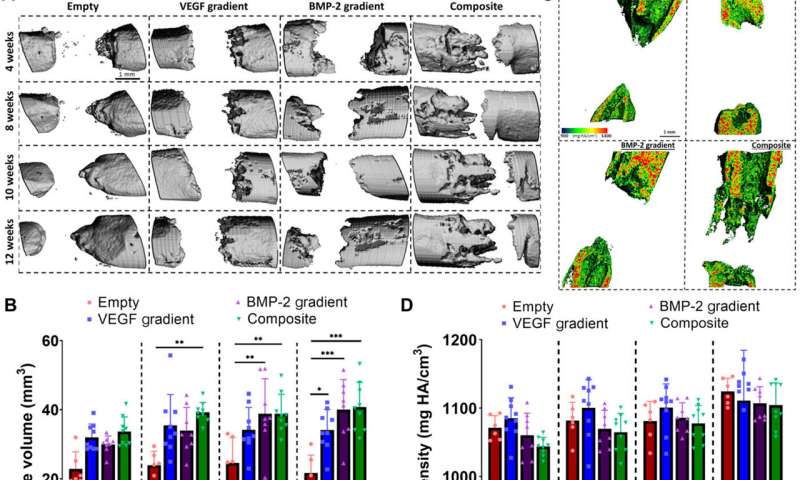
Enhancing angiogenesis within large bone defects
Freeman et al. next demonstrated the spatiotemporal delivery of growth factors (VEGF and BMP-2) to enhance angiogenesis. Using delayed-release BMP-2 constructs containing spatial gradients in VEGF, they recorded enhanced bone formation and blood vessel growth within critically sized rat femoral bone defects. Two weeks after implantation, micro-computed tomography (micro-CT) angiograms showed the appearance of vascular networks in all experimental groups used in the study, alongside primitive immature blood vessels with notable differences between different experimental constructs. Two weeks after surgery, they also noted positive staining for cartilage and new bone in BMP-2 gradient and composite experimental groups. When they conducted microCT tests to understand bone formation, they noted consistent healing patterns. Comparative bone density maps obtained within 12 weeks post-implantation revealed the new bones to contain cortical-like bone comparable to the adjacent native bone. To investigate heterotopic bone formation, the scientists conducted bone volume analysis in a region of interest on the 12 week of reconstruction, where bone preferentially formed in the annulus of the defect with little ectopic bone formation in all experimental groups. Additional histological staining revealed the predominant formation of fibrous tissue, bone marrow and cartilage.
Source: Read Full Article






