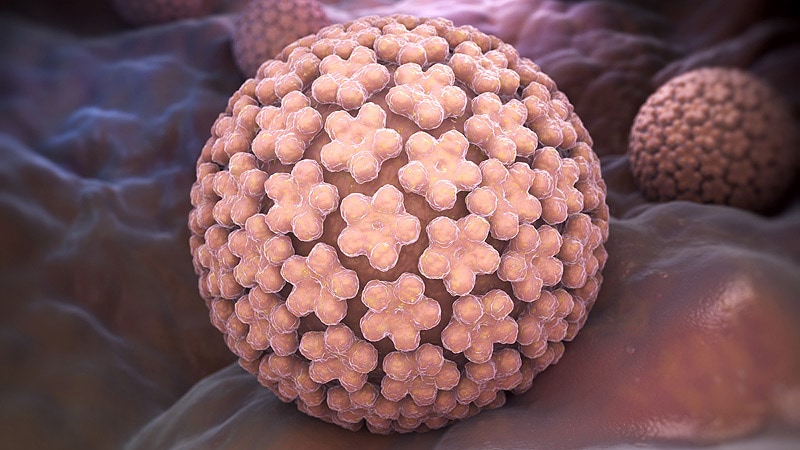
MONTROUGE, France — Four in five women will be infected by one or more human papillomavirus (HPV) strains during their lifetimes. For most of these women, the HPV will be cleared from the body, but 5% of them will develop precancerous lesions in the cervix. The role of vaginal flora in persistent HPV has been brought into focus by research studies carried out over the past few years.
At a press conference ahead of the 46th meeting of the French Colposcopy and Cervical and Vaginal Diseases Society (SFCPCV), Julia Maruani, MD, a medical gynecologist in Marseille, took the opportunity to discuss the importance of vaginal flora and the need to treat cases of bacterial vaginosis.
Striking a Balance
Essential for reducing the risk of sexually transmitted infections (STIs), a healthy vaginal flora is made up of millions of microorganisms, mainly lactobacilli, as well as other bacteria (Gardnerella vaginalis, Atopobium vaginae, prevotella, streptococcus, gonococcus), HPV, and fungi.
Lactobacilli produce lactic acid, which reduces the vagina’s pH, as well as hydrogen peroxide, which is toxic to the other bacteria.
Different factors, such as alcohol, a diet rich in polyunsaturated fatty acids and sugar, and especially smoking, can lead to an imbalance of the bacteria in the vaginal flora and thus result in vaginosis. What occurs is an abnormal multiplication of different types of anaerobic bacteria that are normally present in much lower numbers. There is a relative reduction in lactobacilli, which results in an increased vaginal pH, a greater risk of contracting an STI, and reduced clearance of the HPV infection. “Women who smoke probably experience persistent HPV infections due to an imbalance in vaginal flora,” said Maruani.
Vaginosis and HPV
When there are fewer lactobacilli than there should be, these bacteria can no longer protect the vaginal mucosa, which is disrupted by other bacteria. “HPV then has access to the basal cells,” said Maruani, acknowledging that the relationship between bacterial vaginosis and persistent HPV infections has been the subject of numerous research studies over the past decade or so. “For years, I would see this same link in my patients. Those with persistent vaginosis were also the ones with persistent HPV. And I’m not the only one to notice this. Studies have also been carried out investigating this exact correlation,” she added.
These studies have shown that HPV infections persist in cases of vaginosis, resulting in the appearance of epithelial lesions. Additionally, the lesions are more severe when dysbiosis is more severe.
What about probiotics? Can they treat dysbiosis and an HPV infection at the same time? “Probiotics work very well for vaginosis, provided they are used for a long time. We know that they lessen HPV infections and low-grade lesions,” said Maruani, although no randomized studies support this conclusion. “It’s not a one size fits all. We aren’t about to treat patients with precancerous lesions with probiotics.” There are currently no data concerning the efficacy of probiotics on high-grade lesions. These days, Maruani has been thinking about a new issue: the benefit of diagnosing cases of asymptomatic vaginosis — because treating them would reduce the risk of persistent HPV infection.
This article was translated from the Medscape French edition.
For more news, follow Medscape on Facebook, Twitter, Instagram, YouTube, and LinkedIn
Source: Read Full Article