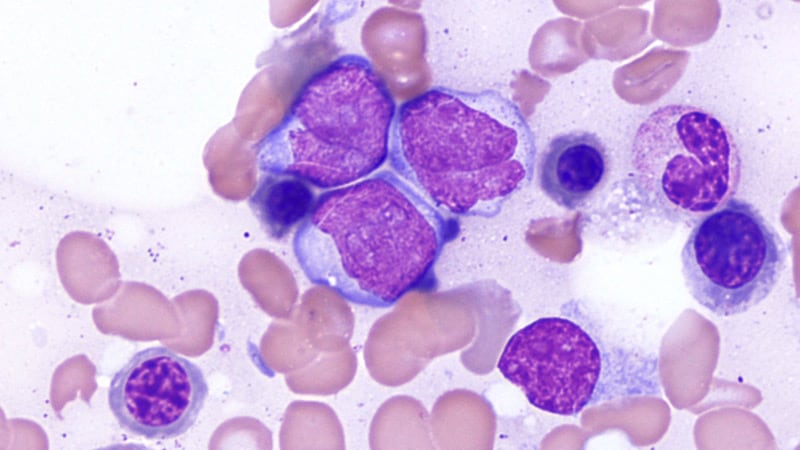
NEW ORLEANS — Investigators confessed to being “astonished” by results of a randomized trial showing that patients with acute myeloid leukemia who have a poor response following induction therapy do just as well going on to immediate allogeneic transplant as they would if they had received an intensive salvage induction regimen to get them into remission before transplant.
The results come from the phase 3 ASAP Trial and were presented here at the American Society of Hematology annual meeting.
“We selected this to be in the plenary because it completely changes how we’ve traditionally thought about acute myeloid leukemia,” commented press briefing moderator Mikkael A. Sekeres, MD, from the University of Miami Miller School of Medicine, who also serves as chair of the ASH Committee on Communications.
“When we have a patient who has relapsed or refractory AML, that person is in a very, very difficult situation, and the mortality among those sort of patients is incredibly high,” Sekeres commented. “So traditionally we’ve given them very high doses of chemotherapy to try to reduce the tumor burden — at least that’s been the theory — to then get them successfully to a transplant.”
This new finding “completely upends that, if these results hold,” he said. The clinical implication is that “we no longer have to hospitalize these patients and give them very aggressive chemotherapy…[and] we don’t introduce all the morbidity from giving them very high dose chemotherapy, which can actually prevent a transplant from happening if they get sick enough, and we can get them to a transplant quicker.”
The ASAP trial was conducted in patients with an unfavorable risk AML who either had a poor response to first induction therapy or a relapse after first induction therapy.
They were randomly assigned to either a remission-induction strategy aiming for a better response prior to an allogeneic hematopoietic stem cell transplant (alloHCT), or a disease-control strategy consisting primarily of watchful waiting with low-dose cytarabine and single doses of mitoxantrone as needed, followed by sequential conditioning and alloHCT.
The results after 4 years of follow-up showed no differences in either leukemia-free survival or overall survival between patients who underwent additional chemotherapy with the remission-induction strategy and those who went straight to transplant, reported Johannes Schetelig, MD, MSc, from the Clinical Trials Unit at DKMS in Dresden, Germany.
“We expected non-inferiority — this was what we tested, and of course this was based on an assumption that we could get close or even somewhat better with respect to the primary endpoint, disease-free survival, after transplantation,” he said.
“What we did not expect is that the early success, [complete response] on day 56 after transplantation, also translates into equal long-term benefit, so this is what I was really astonished about,” Schetelig said at a press briefing prior to his presentation.
Less Intensive Approach
Schetelig explained that the rationale for the study was previous work by his group and others showing that alloHCT in patients with residual aplasia after first induction is feasible, with favorable outcomes compared with standard of care, and also on evidence that sequential conditioning based on high-dose cytarabine or melphalan plus reduced-intensity conditioning and alloHCT resulted in long-term control for relapsed or refractory AML.
He also gave details of the two treatment arms of the ASAP trial. The remission-inducing arm consisted of cytarabine (3 g/m2 for younger patients or 1 g/m2 for patients over age 60) twice daily on days 1-3 plus 10 mitoxantrone mg/m2 on days 3-5 and subsequent alloHCT. In the other group — disease control prior to sequential conditioning and alloHCT — watchful waiting was recommended, but low-dose cytarabine (LDAC) and single doses of mitoxantrone were permitted for disease control.
Although, as Schetelig noted, the statistical goal of the study was to show non-inferiority of the disease control arm, this less intensive strategy succeeded expectations for meeting the primary endpoint of disease-free survival (DFS; a maintained complete response) by day 56 after alloHCT.
In an intention-to-treat and per-protocol analysis, the respective rates of DFS at 56 days in the disease control group were 83.5% and 84.1%. In comparison, the respective rates in the remission-induction group were 81% and 81.3%.
In addition, after a median follow-up from randomization of 37 months, there were no differences in either leukemia-free survival or overall survival out to 4 years after DFS at day 56.
The disease-control strategy was also associated with significantly fewer adverse events grade 3 or greater (23% vs 64%, P < .001), and fewer days in hospital prior to transplant (mean 19 vs. 42, P < .001). There were no significant differences between the trial arms in either deaths within 28 days of randomization or time to discharge from hospital (28 days in each arm).
“These data support sequential conditioning and alloHCT without prior remission-induction chemotherapy whenever a stem cell donor is readily available,” the researchers concluded.
“These results underline the importance of facilitating alloHCT as [the] most effective anti-leukemic therapy in patients with [relapsed or refractory] AML and stress the need for starting donor search at diagnosis,” they added.
The study was sponsored by DKMS gemeinnützige GmbH. Schetelig disclosed honoraria from BeiGene, BMS, Janssen, AstraZeneca, AbbVie, and DKMS. Sekkeres reported no relevant financial relationships.
American Society of Hematology (ASH) 2022 Annual Meeting: Abstract 4. Presented December 10, 2022.
Neil Osterweil, an award-winning medical journalist, is a long-standing and frequent contributor to Medscape.
For more from Medscape Oncology, join us on Twitter and Facebook
Source: Read Full Article